data photo
Since the COVID-19 pandemic swept the world in early 2020, as of May 11, more than 6.23 million people have died from this new infection.
During the same period, the number of infected with COVID-19 reached 498.6 million, approaching 500 million.
The fatality rate, which is the ratio of deaths to confirmed cases, is 1.2%.
Conversely, it means that 98.8% of the infected survived.
In fact, the severity of COVID-19 varies from person to person.
Some asymptomatic infections pass without even knowing that they are infected, while others suffer from acute pneumonia, etc.
Corona 19 patients who have reached severe disease have a relatively greater risk of serious sequelae, even if fortunately they survive.
Why on earth does this discrepancy exist?
According to the research conducted so far, there is no disagreement that the elderly with underlying diseases such as cardiovascular system are at high risk.
However, it is difficult to say that a clear answer has yet to be found.
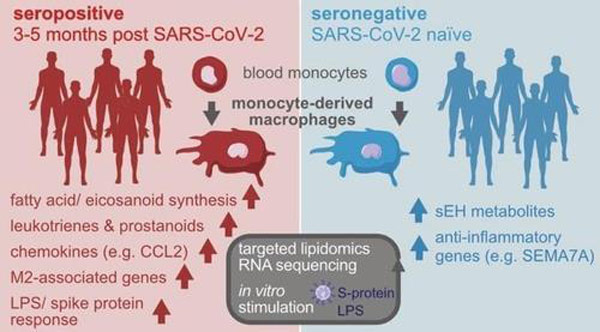
Corona 19 and macrophage action [카롤린스카 의대 등 연구진, 2022년 3월 저널 ‘점막 면역학’ 논문 캡처]
Boston University scientists have published a new study that explains the difference in the severity of COVID-19.
There are different types of macrophages in the lungs, so the severity varies depending on whether the type is well balanced.
The results of this research conducted by scientists at Boston University’s ‘National Institute of Emerging Infectious Diseases’ were recently published as a thesis in ‘Cell Report’, an international life science journal.
According to the outline of the paper published on the website of the American Association for the Advancement of Science, macrophages, a type of white blood cell, play a key role in wound healing.
Macrophages also perform phagocytosis, engulfing and digesting anything that appears to have invaded from the outside, including dead cells, bacteria, and viruses.
However, this aggressive behavior of macrophages is like a ‘double-edged sword’.
It is essential to keeping our body healthy, but it is also involved in the progression of COVID-19 to severe disease.
In fact, there is scientific evidence to show that many COVID-19 deaths are due to an overactive immune response.
The unbridled macrophages attack their own tissues instead of the novel coronavirus.
Then, an excessive immune response causes serious damage to tissues such as the heart and lungs.
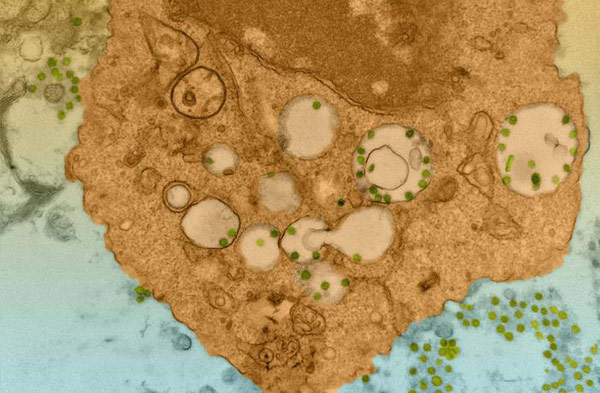
Novel coronavirus that infects lung macrophages [미국 보스턴대 Douam and Kenney, 하버드의대 전자현미경 설비 협조]
A team of researchers from Boston University has developed a mouse model that has been engineered to produce human lung tissue with special conditions and also display a human immune response.
This is to observe what happens at each stage in the lungs of COVID-19 patients.
Knowledge of how the lungs are ruined when COVID-19 becomes critical is largely from autopsies of deceased patients.
However, direct observation or examination of the lungs is difficult in asymptomatic people or people with mild and moderate infections.
As a result of the experiment, no new coronavirus was found in the lungs of mice with normal human immune systems.
It suggests that something protected the mice’s lung tissue from virus attack.
The main character is macrophages, precisely M2 macrophages that reduce inflammation and repair tissues.
However, M1 macrophages that respond to viruses and bacteria promote inflammation in the opposite way.
Mice with severe lung damage from COVID-19 had poor macrophage diversity and a poor balance between types.
In contrast, the lungs of mice with an adequate mix of M1 and M2 macrophages survived viral attack.
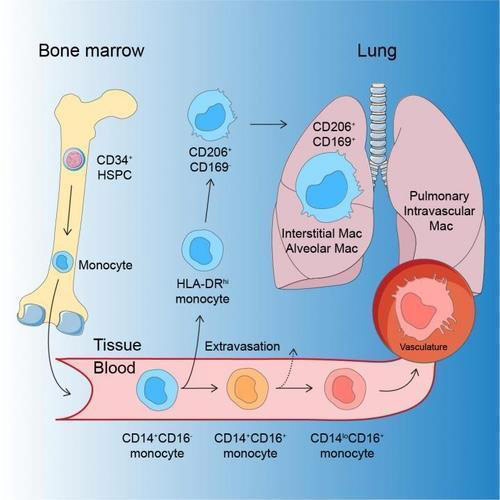
Lung macrophage development process [스웨덴 카롤린스카 의대]
The research team found a set of 11 genes associated with a well-balanced, positive antiviral response in macrophages and named them ‘protection-limited genes’.
When these genes were expressed, macrophages protected lung tissue with a balanced immune response.
This discovery is expected to be of great help in the development of new immunotherapeutic agents for use in COVID-19 patients in the future.
In the paper, the research team emphasized, “Over time, viruses will avoid self-targeting drugs.
This means developing drugs that help COVID-19 patients balance their immune responses can complement current treatment strategies that directly target the virus.