There are more than 100 sub-mutations of the Omicron.
Since the outbreak of pneumonia of unknown cause in Wuhan, Hubei Province, China on December 31, 2019, the coronavirus has undergone alpha mutation, beta mutation, delta mutation, etc. The coronavirus, which has been afflicting mankind for more than three years, still shows no sign of ending. This is because coronaviruses not only have mutations, but also have many sub-displacements derived from each mutation. As of August 2022, more than 130 sub-mutations of the micron are reported.
Why do omicron mutations spread so quickly?
At present, despite the fact that many people are already vaccinated, the omicron submutant BA has been diagnosed worldwide, mainly in Europe. 4 and BA. 5 is steadily increasing. Why do omicron submutations spread so quickly?
BA. The 5 mutation became the dominant species. © Getty Images/loops7
Omicrons, as well as usually new sub-variants of any virus, evolve by changing the function or mechanism of action of the virus. Typically, these variants increase the rate of infection or disease severity (or together). Now that delta and omicron mutations are in turn the dominant strains of coronavirus, scientists are starting to understand these mutations.
First, each mutation has different characteristics due to a specific mutation. For example, delta mutations are more lethal and micron mutations are more contagious. It depends on how the coronavirus gets into cells and how our immune system fights it off.
Omicron is good at evading from our immune system.
A recent study led by Dr. Saathvik R. Kannan and Dr. Austin N. Spratt of the University of Missouri found that omicron mutations might make our immune system better It has been shown to be highly contagious because it can be avoided.
Antibodies from vaccination or infection circulate in our body, preparing to hunt down the virus. When our body detects a coronavirus through its spike protein, it signals the immune system to neutralize the virus. However, the spike protein structure (the part where the antibody binds to the spike protein is mutated) of the micron submutation (BA. To be able to avoid it), a mutation occurred and the top part was changed. Because of this, the antibodies in the body are not good at hunting and destroying the omicron virus particles.
As a result, the avoidance induced by the spike protein structure provoked a rapid increase in infection following omicron mutations were first identified in South Africa in November 2021.
BA. The 5 mutation became the dominant species. © University of Utah Health
For reference, according to Prof. Adrian Esterman, who studies biostatistics and epidemiology at the University of South Australia, the basic reproduction number, a variable indicating the rate at which an infectious disease spreads, is caused by a vaccine or previous infection. The number of infections in the non-immune population) was 9.5 microns for the BA.1 mutation, compared to 9.5 for BA. 2 is BA. It is said to represent 13.3, which is 1.4 times more contagious than 1. On the other hand, BA. 4 and BA. 5 is 18.6, which shows a significantly higher basal infection reproduction number compared to Wuhan strain 3.3 and delta 5.1. BA. 4 and BA. 5 shows the highest basic infection reproduction rate in human history. (Previous highest basic infection reproduction number: basic infection reproduction number of measles virus 16-18)
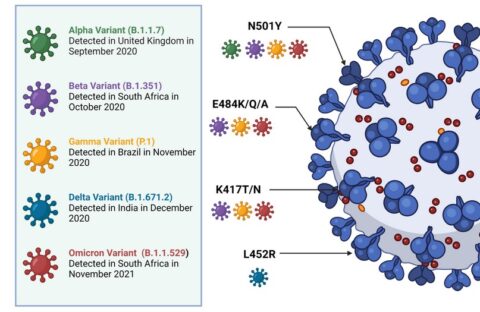
Comparison of differences between SARS-CoV-2 variants © Ordoñez et al. 2022
Delta mutations are more lethal
So, what makes delta more lethal? Due to the recent rise in omicron and centaur mutations, many people have forgotten regarding the delta mutation, but the delta mutation is the most lethal coronavirus. It caused more severe symptoms and increased mortality among infected patients. Recent UK statistics show that the risk of death from omicron mutations is 67% lower than for delta infections.
Delta’s lethality is due to mutations in the spike protein, a viral surface bump, according to a recent US research team led by Dr. Casey Patrick of the University of Colorado Anschutz Medical Campus. This is because two mutations occur in the mutant’s spike protein, which greatly increases the spike protein’s expression. When a virus enters our body, a protein called ACE2 acts as a doorway into our body cells. A mutation expressed in the delta variant tricks ACE2 into allowing it to enter the cell, just as a door usually requires a key when it is closed.
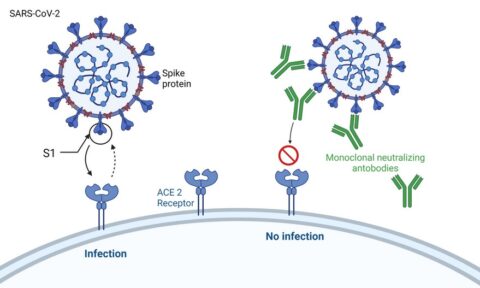
Neutralizing antibodies prevent SARS-CoV-2 from binding to ACE2 and consequently reduce the effectiveness of ACE2. © Ordoñez et al. 2022
Once the virus gets the key and enters the body, it replicates itself and spreads. Therefore, from a biological point of view, the most important variable in lethality may be the number of spike proteins that can bind to ACE2. As described above, in the case of delta mutation, there are many spike proteins, so the probability of entering and multiplying cells is increased, and a larger amount of coronavirus naturally occurs in the body.
When the team looked at how the mutation affects the immune system’s ability to neutralize the virus, the team found that the delta mutation reduced the protein binding of the body’s antibodies to the virus. This naturally leads to higher infection rates and worse symptoms.
Future vaccines should be able to fight new strains
The coronavirus vaccine is rated as having more than half the success in reducing mortality and severe symptoms worldwide, despite numerous side effects. However, as many strains of the coronavirus have now appeared, there is no guarantee that it will not be the case in the future.
As normal viruses evolve in ways that make them more contagious or more lethal (or both), scientists are taking steps to develop new coronavirus vaccines that train our immune systems to cope with new strains. have. According to Dr. Krishna MG Mallela of Dr. Patrick’s research team, there are regarding 220 vaccine candidates in clinical trials worldwide. Malera explained that the new vaccine will help create an immune response that is better suited to dealing with multiple mutations. For example, a team of researchers from the United States and the United Kingdom recently demonstrated a novel vaccine technique once morest novel coronavirus variants such as Omicron, which uses novel nanoparticle technology to easily adapt a targeting process to the variant.
(94)



