Interleukin-13 stimulates mucus secretion, inhibits the whole process of infection
Effective in blocking severe progression such as lung infection
University of North Carolina Medical School, US Proceedings of the National Academy of Sciences
Airway epithelial cells observed under an electron microscope.
Healthy cells (pink), mucus (green), and infected cells that have entered the process of apoptosis (blue) are clearly distinguished.
[미국 노스캐롤라이나 의대 에레 교수 랩 제공. 재판매 및 DB 금지]
(Seoul = Yonhap News) Reporter Ki-cheon Han = The Omicron mutation of the novel coronavirus (SARS-CoV-2) is more contagious than the existing mutation, but the symptoms of infection are not severe.
In fact, even if people are infected with the Omicron mutation, most of them have only mild symptoms similar to a cold or moderate symptoms similar to the flu, and many pass asymptomatically.
This does not mean, however, that there are no deaths from omicron mutations.
Omicron mutations, which spread very quickly, can spread deep into lung tissue and cause serious infections.
In the United States, thousands of people have died from Omicron infection this year alone.
However, as the omicron mutation became the dominant species, an unusual phenomenon was caught in the eyes of scientists.
It is said that allergic asthma patients are exceptionally resistant to omicron infection.
People with this type of asthma are much less likely to progress to severe COVID-19.
Patients with similar chronic diseases, such as chronic obstructive respiratory disease (COPD) or emphysema, have a very high risk of severe COVID-19.
Scientists at the University of North Carolina (UNC) School of Medicine in the United States have figured out the reason for this difference.
Interleukin-13 (IL-13), an inflammatory cytokine (immune protein), played a key role.
IL-13 has been shown to inhibit cellular infection of the novel coronavirus by controlling the expression of ACE2 in host cells.
In order for the novel coronavirus to infect the human body, it must first bind to ACE2 (angiotensin converting enzyme) on the cell surface.
The results of this study, led by Assistant Professor Camille Ehre of the UNC ‘Marsico Lung Institute’, were published in the Proceedings of the National Academy of Sciences (PNAS) of the United States on the 30th of last month (local time).

[미국 노스캐롤라이나대 홈페이지 캡처. 재판매 및 DB 금지]
Professor Ere, who is the lead author of the paper, said, “Allergic asthma patients do not often get severe even if they are infected with the novel coronavirus.
The name interleukin was given to mean a substance that transmits information between white blood cells, and so far, regarding 10 types of interleukins have been discovered.
IL-13 produced by ‘helper T cell type 2’ (Th2) is known to be involved in tissue inflammation, epithelial cell proliferation, and mucus hypersecretion.
Although the research team confirmed that IL-13 plays a key role in preventing the novel coronavirus infection in asthmatics, they might not use IL-13, which triggers inflammation, as a direct treatment.
A number of health factors play a role in the worsening of the condition of COVID-19 patients. Of course, this includes chronic lung diseases such as COPD.
In that respect, it was very interesting that allergic asthma patients who overreact to antigens such as mold, pollen, and animal hair were exceptionally strong once morest COVID-19.
The research team first investigated the mechanism of excretion of foreign substances from airway epithelial cells.
Analysis of the gene sequence of airway epithelial cells infected with the novel coronavirus revealed a specificity in the ACE2 receptor.
According to the expression level of ACE2, the type of infected cell and the viral load following infection vary.
The escape of the virus from the ciliary cells of the mucus-covered airway epithelium was also observed through electron microscopy.
In addition, it was confirmed that viral infection causes severe pathological changes in cells.
At the peak of the accumulation of these changes, the ciliary cells filled with virus particles trapped in the mucus were even detached from the airway surface.
Professor Ere explained, “The escaped ciliate cells can become a kind of virus reservoir and help spread and spread,” adding, “In addition, the possibility of spreading the infected cells deep into the lung tissue can increase.”
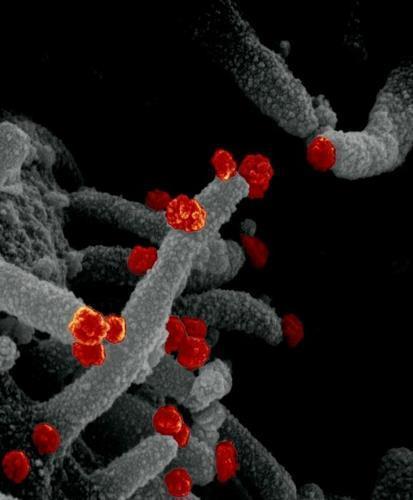
A scanning electron microscope image of the novel coronavirus (red) emerging from the surface of cultured cells.
[미국 NIAID(국립 알레르기 감염병 연구소). 재판매 및 DB 금지]
Perhaps because it is often used to entrap invading viruses, the infected airway epithelial cells lacked the major mucin protein (MUC5AC).
However, the viral load continued to increase. This is because the viral infection has progressed so violently that it overwhelms the cells that secrete the mucus protein.
The research team noted that this mucus protein was excessively secreted even in patients with allergic asthma.
It was also known that IL-13 stimulates the secretion of mucous proteins in the lungs when asthmatics are exposed to allergens.
The research team applied IL-13 to human airway epithelial cells to create a model similar to the airway of asthma patients.
Then, viral titer, mRNA level, ciliary cell exit rate, and total number of infected cells were measured.
Surprisingly, however, all figures were found to have dropped significantly. Even if the mucus was completely removed from the airway epithelial cells, there was no change in the lowered level.
This suggests that other factors play a role in IL-13’s protective effect once morest the novel coronavirus.
The question was solved by mass RNA sequencing.
It was IL-13 that up-regulates control genes such as glycoprotein synthesis, ion transport, and antiviral processes that are important for immune defense of the airways.
IL-13 also decreased the expression of ACE2 and was involved in suppressing intracellular viral load and intercellular propagation.
In a word, IL-13 had a great effect on the entire process from the invasion of virus cells to proliferation following penetration and propagation following proliferation.
This action of IL-13 consequently prevented the novel coronavirus from causing serious lung infections.
“We reaffirmed the need to treat people infected with the novel coronavirus as early as possible to prevent them from progressing to severe disease,” Ere said.
Report on Kakao Talk okjebo
<저작권자(c) 연합뉴스,
Unauthorized reproduction-redistribution prohibited>
2022/04/01 18:00 Send