In order to illustrate the impact of the Covid-19 crisis and to decipher the state of mental health of healthcare personnel in France, Hublo, a player in replacement solutions in healthcare establishments, carried out a study with more than 22,600 healthcare professionals to quantify well-being at work in healthcare establishments. The feeling of disillusionment among caregivers seems to deepen following only 3 years of experience.
The majority of survey participants believe that their well-being is not considered a priority by the health sector. Among them, 96% of State Registered Nurses (IDE) rate this level of priority below 6/10. However, 70% of caregivers surveyed indicate that healthcare establishments must prioritize their well-being if they wish to recruit them or see them stay.
“I’m tired of hearing regarding a shortage of staff, because we had it and we mightn’t retain it, because of the poor working conditions and now it’s hard to recruit for the same cause! (…) That’s how we created the shortage of caregivers. Because because of this suffering at work, the nursing staff preferred to change jobs, out of spite”.
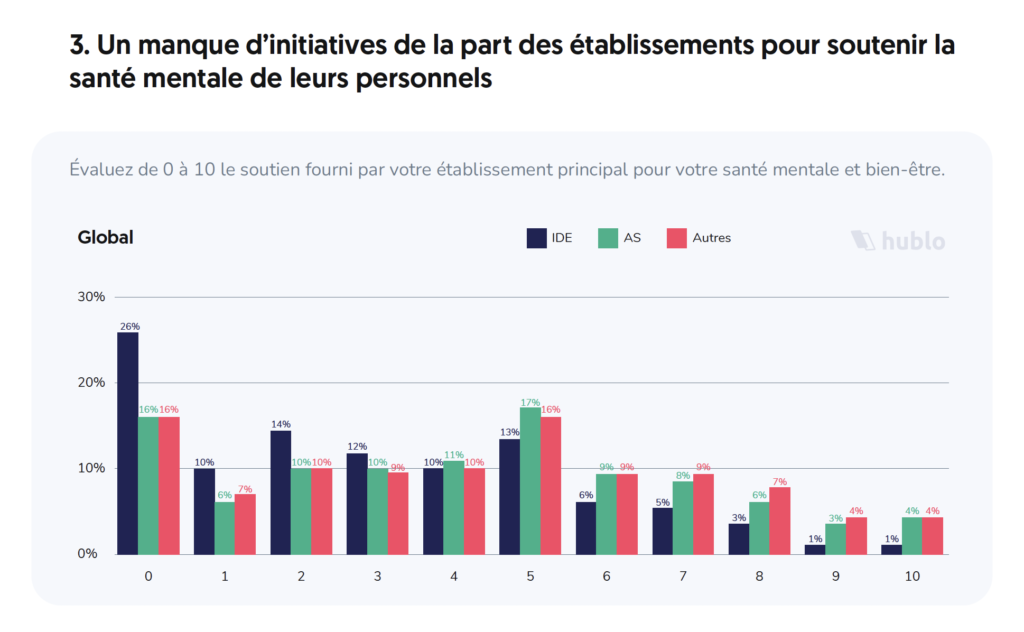
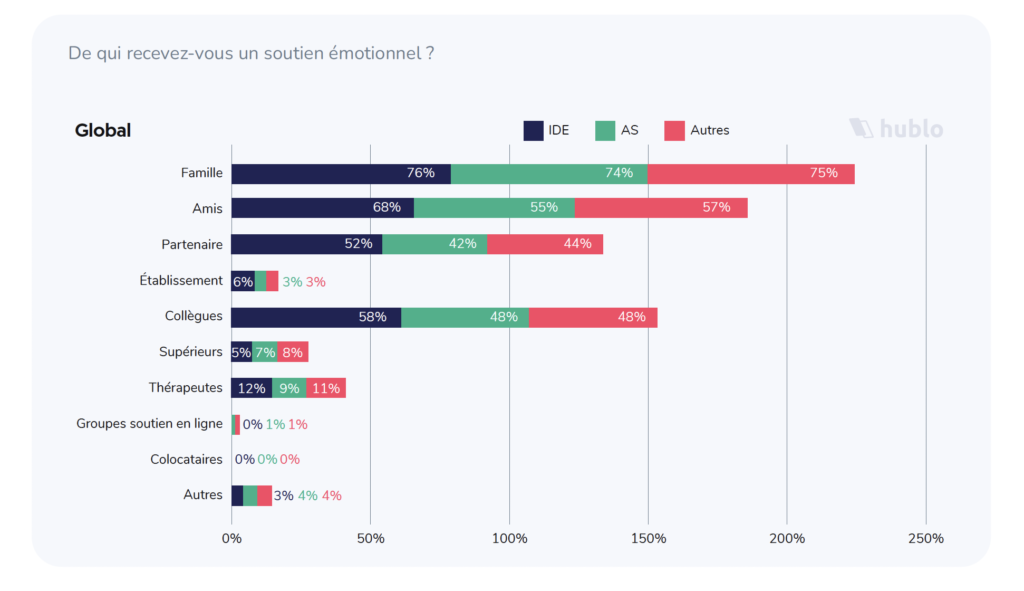
The study also reveals that the work establishment and management are generally not seen as a source of support at all. In public hospitals, only 0.4% of IDEs and 1% of nursing auxiliaries feel that they are emotionally supported by their establishment, while family, partners and colleagues are a significant source of support for the majority of them. Moreover, more than 25% of public hospital nurses feel that they receive absolutely no support from their establishment, a symbol of deep disappointment with the health system.
A caregiver laments an imposed à la carte schedule, the schedules change the day before or even during the day ».
Another has “the impression of being only a box in the schedules, that the future will not bring any evolution, and that when we make proposalsions de solution to improve the quality and the workload, we are not taken into consideration”.
Improving management appears to be the decisive factor in retaining caregivers.
The study also reports on omnipresent stress at work, for which the lack of personnel is systematically singled out first. The workload is also considered too heavy by one out of two caregivers. Communication with superiors is also singled out since it is cited by more than a third of caregivers surveyed as the main stress factor. To overcome this and thus improve well-being at work, all the caregivers questioned ask for better communication between management and the teams. In addition, more than two thirds of caregivers and other paramedical staff, and 71% of FDIs, consider that the lack of recognition is the main reason that might lead them to change jobs.
“Always more tasks to do with the same time available” and, therefore, the “lack of time for quality care”.
Les chiffres clés de l’étude - Moins de 5% des soignants s’estiment soutenus sur le plan émotionnel par leur établissement. - Le manque de personnel est cité comme facteur de stress principal au travail par plus de 81% des répondants. - Plus d’un tiers des soignants interrogés indiquent que la communication avec les stress principaux au travail. - Le sentiment de désillusion des soignants semble se creuser après 3 années d’expérience. - Plus d’un tiers des Infirmiers Diplômés d’État ne comptent pas exercer leur métier toute leur vie. - 50% des soignants interrogés considèrent que le stress au quotidien est l’un des facteurs majeurs qui impactent négativement leur bien-être au travail.
• Survey on the well-being and mental health of caregivers in France. Between exhaustion and disaffection: how are caregivers really doing? hublo, press release, February 2022. Image and infographic credits, hublo.




