From one moment to the next, the person begins to feel tired, confused, sleepy and disoriented.
At first glance, symptoms like these suggest that something is not right in the brain and dementia seems to be gaining ground.
However, for a considerable number of patients, these ailments are related to problems in another part of the body: the liver.
Although little known, the hepatic encephalopathy attracts the attention of specialists, who are concerned about the lack of an adequate diagnosis of the disease and the probability of an increase in the number of people affected in the coming years, due to the Increase in obesity and other diseases that affect metabolism.
But there is good news: This cause of cognitive decline can be reversed with small adjustments in routine and the help of some medications.
More common than it seems
A study published in late June in The American Journal of Medicine revealed that hepatic encephalopathy may be more common than previously thought.
Researchers at Virginia Commonwealth University and the Richmond Veterans Affairs Medical Center in the United States analyzed data collected between 2009 and 2019 from 68,807 patients diagnosed with dementia.
The results of Tests that assess liver health (known by the acronym FIB-4)) revealed that 12.8% of these individuals presented suggestive indicators of cirrhosis and potentially suffered from hepatic encephalopathy.
The percentage is similar to that of another survey conducted by the same group of scientists. In a study of 177,000 American veterans, about 10% of them showed changes indicating liver dysfunction.
“FIB-4 is a simple method to determine the risk of advanced liver disease. Patients with changes in this test have a high probability of having cirrhosisa condition that does not usually present many symptoms,” explains Dr. Jasmohan Bajaj, one of the authors of the study.
“And more than half of patients with cirrhosis develop some form of hepatic encephalopathy,” he says.

Bajaj points out that he himself followed cases of people who had been diagnosed some type of dementia (such as Alzheimer’s) or Parkinson’s diseasebut who actually had liver problems.
In these episodes, it was enough to make the correct diagnosis and start treatment for the neurological and cognitive symptoms to completely resolve.
For Dr. Sonia Brucki, coordinator of the Cognitive and Behavioral Neurology Group at the Hospital de Clínicas in Sao Paulo, it is striking that American specialists have found changes suggestive of hepatic encephalopathy in almost 13% of patients with dementia.
“Also because liver function tests are mandatory when investigating any cognitive impairment,” he says.
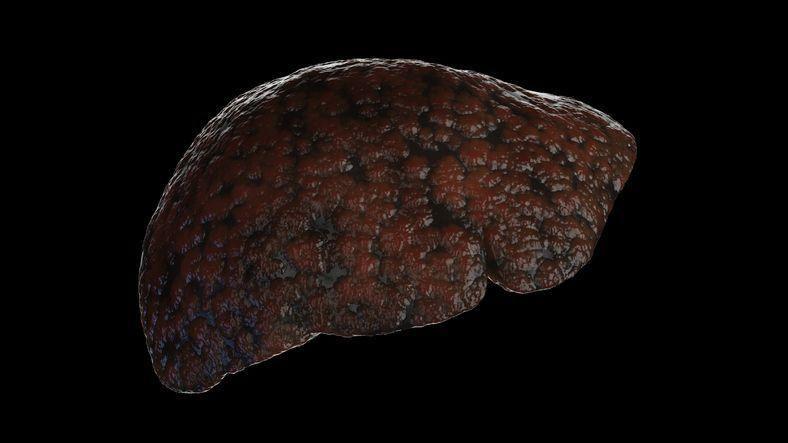
Broken liver
Hepatologist Raymundo Paraná, professor at the Federal University of Bahia, explains that hepatic encephalopathy is a brain poisoning by substances that should have been metabolized by the liver.
It is worth remembering that the liver is essential in the digestion process and also “degrades” or metabolizes toxic elements that can be harmful to the rest of the body. These molecules are then eliminated in urine or feces.
When the liver is diseased and damaged by a virus (such as those that cause hepatitis B y C), excess fat, alcohol or other harmful substances, stops working as expected.
Consequently, Certain molecules that should be filtered and disposed of remain in the body and may end up in the brain.where attention, reasoning and memory will be impaired.
“There are cases in which blood flow to the liver is altered.. As a result, blood is diverted to other areas, such as the esophagus and stomach, and reaches the brain without passing through the liver tissue,” explains Paraná.
The doctor points out that Hepatic encephalopathy is a relatively common conditionbut there is some difficulty in detecting subclinical cases, with milder symptoms that can be confused with other diseases.
“In classic cases of the disease, the family begins to notice that the individual presents lethargy and mental confusion, sleep disturbances, loss of sphincter control and hand tremors“, lists Paraná.
“These are very indicative signs of hepatic encephalopathy,” he added.
Brucki insists that Hepatic encephalopathy and “classic” dementia have very different manifestations.
“Liver disease progresses more quickly and is different from dementia, which involves chronic manifestations, with progressive changes in cognitive functions, affecting memory, language, attention and reasoning ability,” he says.
Confusion between the two diseases occurs with the more subtle forms of liver involvement. “The patient may not present tremors or reduced reflexes, which makes diagnosis difficult,” says the specialist.
In these cases, There is a higher risk of receiving a misdiagnosis and then undergo treatment for Alzheimer’s, for example.
In addition to tests that assess liver health, Paraná says your doctor may recommend a electroencephalogram and other imaging tests, which evaluate the accumulation of certain substances in the nervous system.
How to reverse cognitive decline
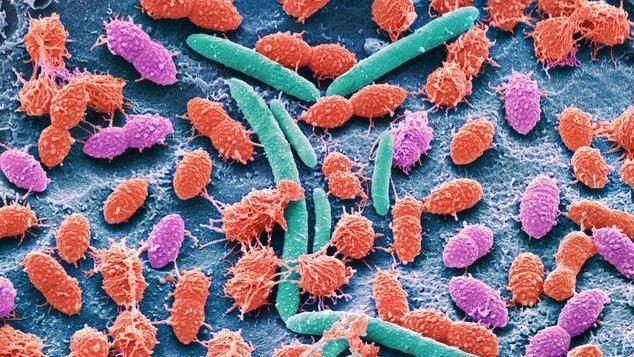
It is curious to think that for a disease that originates in the liver and affects the functioning of the brain, the solution is in a third part of the body: the intestine.
Paraná explains that in the case of hepatic encephalopathy, one of the main substances that “escape” and generate problems in the nervous system is ammoniaproduced largely by bacteria that inhabit the digestive system.
“Normally, ammonia passes to the liver, where it is transformed into urea and eliminated in urine,” he says.
In this group of patients, Excess ammonia ends up in the head, where it “poisons” the brain and causes symptoms of mental confusion, tremors and lethargy.
“The aim of the treatment, therefore, is to prevent ammonia from reaching the brain,” Paraná sums up.
To do this, experts can rely on several different strategies.
The first consists of avoid constipation. This is because Constipation stimulates the proliferation of ammonia-producing bacteria in the intestine. and the more ammonia, the greater the brain intoxication.
The main way to prevent a scenario like this is to use lspecific axantswhich guarantees at least two bowel movements a day. After all, along with the feces, millions of bacteria are flushed down the drain.
“Medicines such as lactulose prevent constipation and create an environment in the intestine that makes it difficult to absorb ammonia,” says the hepatologist.
When this first strategy fails, doctors often turn to a drug called Rifaximin, which controls the bacterial population in the intestine.
Paraná also points out that the drugs with diuretic effectused to treat high blood pressure, for example, can stimulate the production of ammonia in the body.
In these patients, it may be necessary to adjust the dose or change the active ingredient to avoid hepatic encephalopathy.
“Also It is important to avoid medications that are metabolized in the liver and to seek a low-protein diet.“, adds Brucki.
All of these measures even reverse cognitive decline related to intoxication of the nervous system.
“Most patients with hepatic encephalopathy respond well to treatment, so it is critical to identify these individuals to prevent their condition from being confused with dementia,” Bajaj said.
Finally, Paraná warns that a series of phenomena that have intensified in recent years could make this situation increasingly common.
“The ageing of the population has led to an increase in chronic and degenerative diseases, some of which affect the liver,” he says.
“In addition, the inappropriate use of medications, herbs and phytotherapeutics, alcohol abuse, the transmission of viral hepatitis and the increase in autoimmune diseases, obesity and metabolic syndrome generate hepatic repercussions.”
The hepatologist reinforces that Several diseases that damage the liver are silent.
Many people, for example, have no idea that they have cirrhosis and only show the first symptoms when the disease is already in an advanced and irreversible stage.
“It is important that every patient undergoes basic investigation, which includes a blood tests and an ultrasoundto know if the liver is sick or not,” he concludes.
Click here to read more stories from BBC News Mundo.
You can also follow us on YouTube, Instagram, TikTok, X, Facebook and on our new channel WhatsAppwhere you’ll find breaking news and our best content.
And remember that you can receive notifications in our app. Download the latest version and activate them.
#reversible #disease #confused #Alzheimers #Parkinsons #occurs #liver #brain



