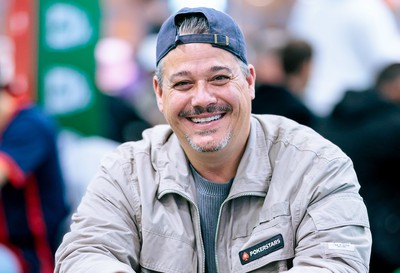
Boston Rob: Back in Love with Poker
‘Survivor’ Star Boston Rob Bets on Poker Comeback DUBLIN, Ireland—Rob Mariano, better known as “Boston Rob” from his multiple appearances on teh reality TV show
‘Survivor’ Star Boston Rob Bets on Poker Comeback DUBLIN, Ireland—Rob Mariano, better known as “Boston Rob” from his multiple appearances on teh reality TV show

Tallahassee, FL – In a shocking turn of events, the suspect accused of a mass shooting at Florida State University (FSU) that left two dead

“`html Cutaneous Leishmaniasis Cases Reported in argentina: What Travelers Need to Know By Archyde.com News Service May 8, 2024 Health officials are monitoring cases of

Headline: AI Voice Cloning Raises Thorny Legal Questions After Indian Singer Wins Landmark Case NEW YORK – A recent court victory by Bollywood playback singer
‘Survivor’ Star Boston Rob Bets on Poker Comeback DUBLIN, Ireland—Rob Mariano, better known as “Boston Rob” from his multiple appearances on teh reality TV show

Tallahassee, FL – In a shocking turn of events, the suspect accused of a mass shooting at Florida State University (FSU) that left two dead

“`html Cutaneous Leishmaniasis Cases Reported in argentina: What Travelers Need to Know By Archyde.com News Service May 8, 2024 Health officials are monitoring cases of

Headline: AI Voice Cloning Raises Thorny Legal Questions After Indian Singer Wins Landmark Case NEW YORK – A recent court victory by Bollywood playback singer

© 2025 All rights reserved