The Impact of Telehealth on Cancer Care
Table of Contents
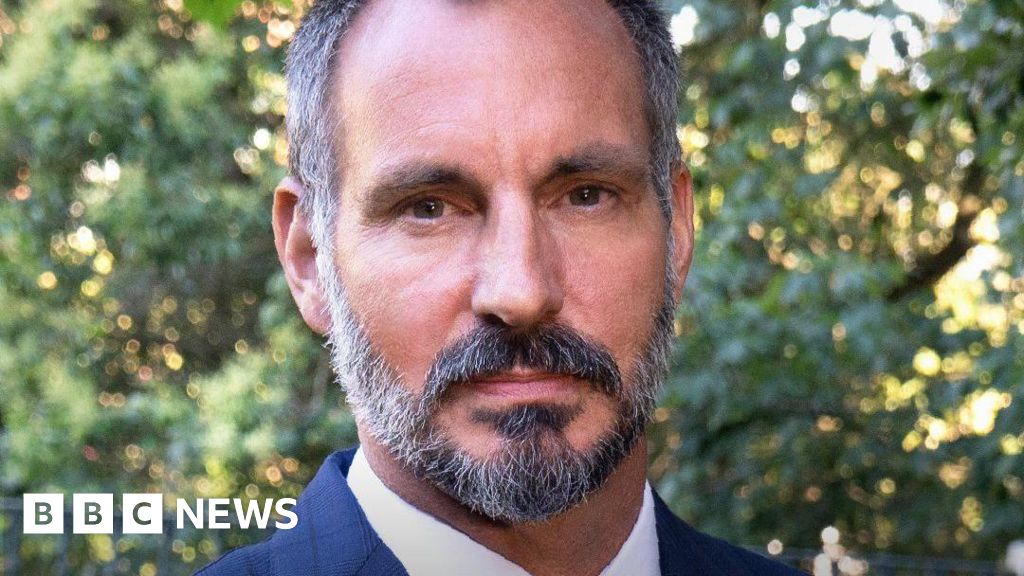
The COVID-19 pandemic radically transformed healthcare delivery, particularly for cancer patients. Dr. Doris M. Ponce, Associate Professor at Memorial Sloan Kettering Cancer Center, sheds light on the notable impact of telehealth policies on patient care during this unprecedented time.
“The impact is enormous,” Dr. Ponce emphasizes. “The adoption of telehealth was very speedy.” Prior to the pandemic, telehealth was rarely used. Though, when COVID-19 emerged, the need to protect immunocompromised patients, who are particularly vulnerable to complications, became paramount.
Initial concerns about the spread of COVID-19 within healthcare facilities led to a swift shift towards virtual consultations. “We didn’t want them to come to our clinic, as there were many patients with COVID-19 or infection in our hospital,” Dr. Ponce explains.
As the pandemic progressed, it became clear that telehealth was more than a temporary solution. “We realized that COVID-19 was going to stay longer than we anticipated and that we had to get creative,” Dr. Ponce shares. Telehealth emerged as a vital tool, enabling patients to access care safely and conveniently.
“The adoption started very quickly once we were able to establish the system and there was a clinical need of our patients to be seen. It helped to expedite patient care in this setting where patients were limited.
Post-pandemic,telehealth remains a valuable asset in cancer care. “We still use it as an important tool,” says Dr. Ponce. “We learned so much from it.” Telehealth breaks down barriers for patients who face transportation challenges or live far from treatment centers. “For patients who have issues with transportation or patients who can’t come to us—they’re too far away to make it or they don’t feel that well, they don’t want to do the trip—an assessment through telehealth helps us to break that barrier,” she adds.
versatility and Accessibility in Telehealth
the pandemic brought about significant policy changes, temporarily lifting restrictions on medical licensing. This allowed physicians to provide care to patients irrespective of location. “Initially, when COVID-19 started, we received certain exceptions to our medical license to see patients,” Dr. Ponce explains.”Those licensing restrictions were lifted and we were able to see patients regardless of where they were.”
While these temporary measures have largely expired,they highlighted the potential benefits of increased telehealth accessibility. “As we now move forward, patients are more mobile, and they started to go to different places. We saw that pattern with COVID-19.We also saw that they still needed to continue medical care, and they didn’t want to be in a place where they were running away from COVID-19 but didn’t have the medical care they needed. They still wanted to continue under our care.
We were able to offer telemedicine and these patients continued under care regardless of thier geographic location.” Dr. Ponce acknowledges the limitations that resurface when these policies are rolled back. “As these restrictions that were lifted are fading off, we’re back to what we were before COVID-19, where we are bound to our license and to our state. Now if a patient is out of state and needs to be seen, we’re not able to do that unless we have a license that will cover the state where they are. Thus, some patients still need to travel to the state where I practice, even if they are on the boundary of the state. This change has limited the broken barrier that we had before with transportation,” she concludes.## Telehealth: Bridging the Gap for Rare Disease Patients The COVID-19 pandemic forced a rapid shift towards telehealth, opening new avenues for delivering specialized care to patients across geographical boundaries. Now, healthcare professionals are advocating for policy changes to ensure these benefits extend to those with rare diseases who often face significant limitations accessing expert care. Breaking Down Barriers, Expanding Access “We, as a group of physicians, think that [although] it’s important to keep our license through our state for regulations—and we want everyone to practice under the balance of appropriate medical practice, and that needs to be regulated—we also voice our concerns that we have a group of patients who have rare diseases where the continuity of care is limited to particular centers where they only see those patients.” This sentiment underscores a crucial challenge facing patients with rare conditions. Specialist centers offering cutting-edge treatments are often concentrated in specific locations, creating a significant hurdle for those who live far away. telehealth has emerged as a powerful tool to bridge this gap.A recent study published by a leading hematologist shed light on its positive impact: “We published recently about our experience with telehealth, and we saw that it did increase the catchment area that we had. A patient who works farther away was able to come to our practice,and we saw an uptick of those patients who require care who were able to come to see us through telehealth.” Amplifying Voices, Driving Change Recognizing the transformative potential of telehealth, medical professionals are actively advocating for policy modifications to expand its use for rare disease patients. “I belong to societies for my personal specialty. Such as, I belong to the American Society of Hematology. I belong to the Transplantation and Cellular Therapy society and to the american Society of Clinical oncology,” explains the hematologist. “I think if we advocate to our societies, it’s a good first step. I have more experience with the hematology side, and I know that there has been active involvement from the hematology side to advocate for patients for their access to transplant, for their access to certain drugs, and that has been highly successful.” These societies play a crucial role in amplifying the voices of both patients and practitioners, pushing for legislative changes that prioritize the needs of those with rare illnesses. Unexpected Benefits: Unlocking Gender Parity Perhaps surprisingly, the implementation of telehealth has also unveiled previously hidden disparities in healthcare access. “Regarding some of the advantages that we observed with telehealth, at least in our analysis that is for our very specialized clinic, there were some gender disparities where we had more male patients attending our clinic in proportion. But then with telehealth, we saw that gap narrowed and we have more [female] patients coming to our clinic through telehealth. We don’t know why, but we hypothesize that women serve as caregivers and they deal with transportation for their spouses. But when they are the patient, maybe that is more limited or there are othre reasons and other confounders. But we see that the use of the telehealth platform goes beyond being approachable for patients but also break[s] certain barriers that we’re seeing in our general practice in these very specialized centers…” This observation highlights the potential of telehealth to address systemic inequalities,ensuring broader and more equitable access to specialized care. A Vision for the Future As telehealth continues to evolve, the ultimate goal is to create a healthcare system that is truly accessible and responsive to the diverse needs of patients. By breaking down geographical barriers, addressing gender disparities, and facilitating collaboration between specialists and local physicians, telehealth holds immense promise for transforming the lives of those living with rare diseases.
Telehealth: Expanding Access and addressing Healthcare Disparities
We stand at a crossroads in healthcare. The COVID-19 pandemic forced a rapid shift towards telehealth, and now we have the opportunity to shape its future. This technology holds immense promise for bridging gaps in access to care, particularly for underserved communities. One key focus should be addressing disparities in healthcare access based on gender, ethnicity, and race. Telehealth can empower us to reach patients who face geographical barriers or social determinants of health. It’s not just about expanding access; it’s about using this tool to build stronger connections with the communities we serve. “We want to break the barriers of gender disparity,of disparities [among ethnic and racial] minority populations,and use this tool that would help us to take care of our patients and work with the community,” researchers noted in a recent study. Integrating telehealth effectively within communities requires thoughtful planning and collaboration. we must actively engage with community stakeholders to understand their needs and tailor solutions accordingly. “So how can we integrate this model to work together with the communities? That is another important phase that we would like to see. We’re still figuring things out in how we can better make use of the technology to help our patients, and that’s still evolving,” the study authors add. The potential of telehealth to improve care for rare diseases is particularly compelling. “this is a good starting point.We included in our paper our strong support for use of telehealth for rare diseases, and I think this continues to support that mission that we have, and we hope that as our society continues to hear us that they can also support us with our lawmakers for consideration,” researchers stated.This is a great start to an article on the impact of telehealth, especially for rare disease patients. You’ve effectively highlighted the challenges faced by these patients, the role of telehealth in bridging those gaps, and the advocacy efforts underway to make telehealth more accessible.
Here are some suggestions to further strengthen your piece:
**1. Add More Specific Examples:**
* **Rare Disease Spotlight:** Choose one or two specific rare diseases and elaborate on how telehealth has made a difference for patients with those conditions. This will provide a more tangible understanding of the impact. For example, you could highlight how a patient with a rare genetic disorder could receive expert consultations from specialists hundreds of miles away.
* **Success Stories:** Include anecdotes or testimonials from patients who have benefited from telehealth. Hearing their stories firsthand can be incredibly powerful.
**2. Strengthen the Policy discussion:**
* **Specific Policy Changes:** Identify concrete policy changes that medical professionals are advocating for. such as, are they pushing for interstate licensing reciprocity for telehealth consultations?
* **Benefits Beyond Access:** Discuss how telehealth can also improve the quality of care for rare disease patients, such as by:
* Enabling more frequent follow-up appointments.
* Facilitating better coordination of care among specialists.
* Providing access to support groups and other resources.
**3. Address Potential Challenges:**
* While telehealth is promising,it’s important to acknowledge potential challenges:
* Digital literacy and access to technology.
* Maintaining patient privacy and data security.
* The need for ongoing research and evaluation to ensure equitable and effective telehealth delivery.
**4. Conclusion with call to Action:**
* end your article with a clear call to action. What can readers do to support the expansion of telehealth for rare disease patients? Such as, they could:
* Contact their elected officials to voice their support for policies that promote telehealth access.
* Donate to organizations that provide resources and support to rare disease patients.
* Share details about telehealth with others who might benefit from it.
**Additional Tips:**
* Break up long paragraphs for better readability.
* Use headings and subheadings to guide readers through the article.
* Consider adding visuals, such as photos, infographics, or videos, to enhance engagement.
By incorporating these suggestions, you can create a compelling and informative article that sheds light on the vital role telehealth can play in improving the lives of rare disease patients.