Dr. Ahmad Ridhoi MSi also explained the structure and mechanism of the HMPV virus via the ITS Medics webinar, Wednesday (15/1)
Kampus ITS, ITS News – Cases of respiratory tract infections caused by Human Metapneumovirus (HMPV) have recently captured public attention due to their striking resemblance to COVID-19 symptoms. To shed light on this emerging health concern, the Sepuluh Nopember Institute of Technology (ITS) hosted a webinar titled ITS Medics on Wednesday, January 15. The event aimed to enhance public understanding of HMPV, its transmission, and preventive measures.
Dr. Ahmad Ridhoi MSi, a prominent speaker at the webinar, opened the session by noting that while HMPV was first identified in 2001, it has only recently gained meaningful attention. This surge in interest stems from its symptomatic similarities to COVID-19, including its impact on the respiratory system. “Though, unlike COVID-19, HMPV does not cause loss of smell or taste,” Ridhoi clarified, emphasizing a key distinction between the two viruses.
Ridhoi further elaborated on the varying effects of HMPV across different patient groups. While healthy adults typically experience mild symptoms such as coughing,fever,nasal congestion,and shortness of breath,the virus can pose a serious threat to vulnerable populations. infants,older adults,and individuals with pre-existing health conditions are at higher risk of developing severe complications,including pneumonia.
In terms of transmission, HMPV shares common pathways with COVID-19. Both viruses spread through direct contact with infected individuals and respiratory droplets released during coughing or sneezing. However, Ridhoi highlighted a critical difference: “Unlike COVID-19, HMPV is not transmitted through aerosols.” This distinction underscores the importance of understanding the unique characteristics of each virus to implement effective preventive measures.
Understanding Human Metapneumovirus: A silent Threat to Respiratory Health
Table of Contents
- 1. Understanding Human Metapneumovirus: A silent Threat to Respiratory Health
- 2. the Role of Neutralizing Antibodies in Combating hMPV
- 3. Prevention strategies: What You Need to Know
- 4. Why hMPV Deserves More Attention
- 5. Conclusion
- 6. The Role of Neutralizing Antibodies in Combating hMPV
- 7. Prevention Strategies: what You Need to Know
- 8. Why hMPV Deserves more Attention
- 9. Understanding Human Metapneumovirus (HMPV): Symptoms, Prevention, and Global Impact
- 10. What is Human Metapneumovirus (HMPV)?
- 11. Who is Most at Risk?
- 12. How to Protect Yourself and Others
- 13. raising Awareness About HMPV
- 14. Conclusion
- 15. Understanding HMPV: A Silent Threat to Respiratory Health
- 16. The Discovery and Unique Traits of HMPV
- 17. Why HMPV Continues to Challenge Public Health
- 18. Prevention and Awareness: The Path Forward
- 19. Understanding Human Metapneumovirus (HMPV): A Persistent respiratory Threat
- 20. What Is HMPV?
- 21. Why HMPV Remains a Challenge
- 22. the Importance of Awareness and prevention
- 23. Conclusion
- 24. What are the primary symptoms of HMPV infection?
- 25. What is Human Metapneumovirus (HMPV)?
- 26. Clinical Presentation and Diagnosis
- 27. Who is Most at Risk?
- 28. Why is HMPV a Growing Concern?
- 29. Prevention and Control Measures
- 30. The Road Ahead: Research and Development
- 31. Conclusion
Table of Contents
As its revelation in 2001, human metapneumovirus (hMPV) has quietly become a major contributor to respiratory infections across the globe. Despite its widespread impact, the medical community still lacks targeted antiviral treatments or vaccines to combat this elusive virus. This gap in solutions underscores the urgent need for greater awareness and research into hMPV.
the Role of Neutralizing Antibodies in Combating hMPV
One promising avenue in the fight against hMPV lies in neutralizing antibodies. These specialized proteins have shown potential in targeting the virus, offering hope for future treatments. However, the development of such therapies remains in its early stages, highlighting the complexity of tackling hMPV effectively.
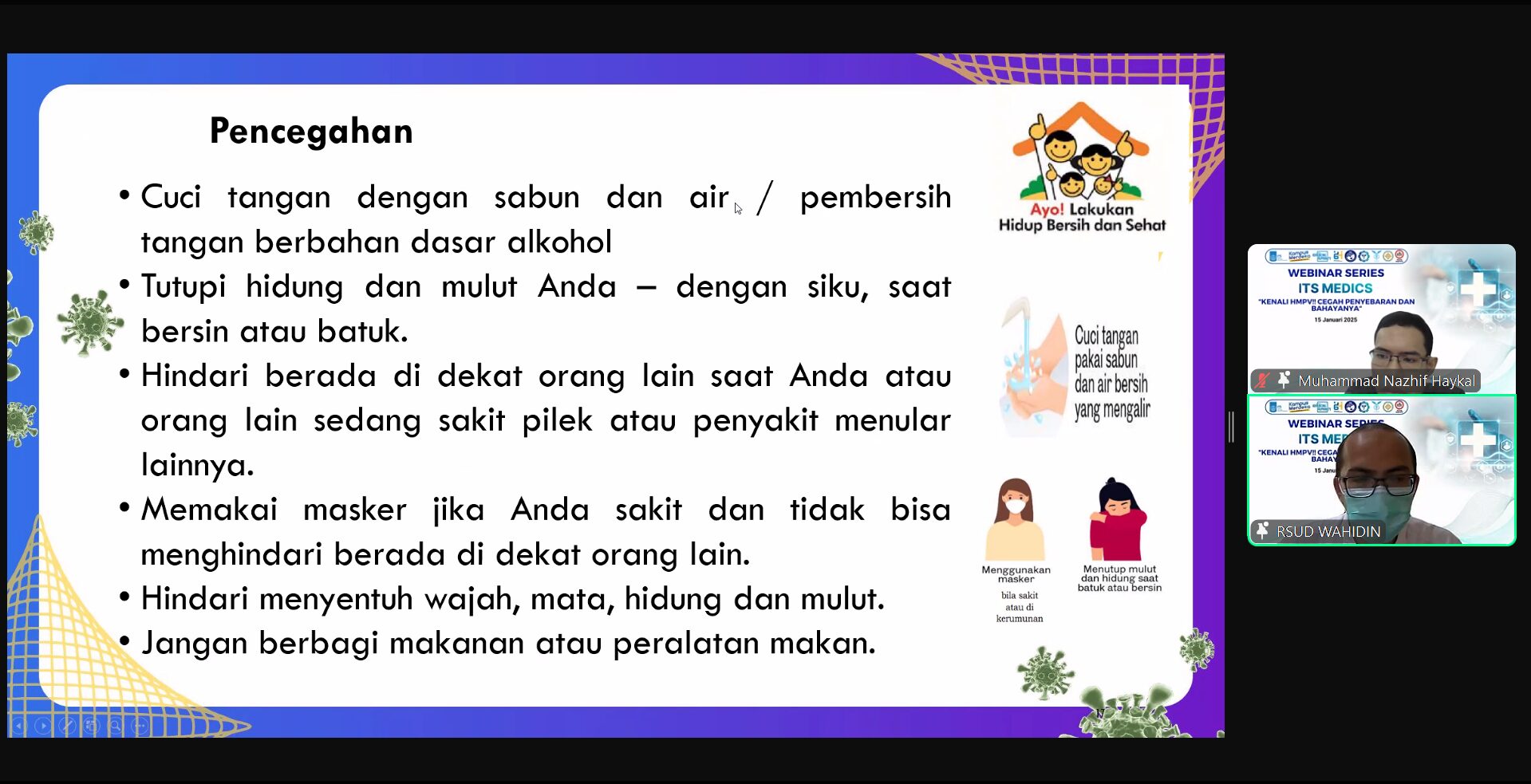
Prevention strategies: What You Need to Know
while medical solutions are still evolving, prevention remains a cornerstone in managing hMPV. Simple yet effective measures, such as frequent handwashing, avoiding close contact with symptomatic individuals, and wearing masks in crowded spaces, can significantly reduce the risk of infection. These practices,familiar from the COVID-19 pandemic,are equally vital in curbing the spread of hMPV.
Why hMPV Deserves More Attention
Despite its important impact on public health, hMPV often flies under the radar. Unlike more widely recognized respiratory viruses, hMPV lacks the same level of public awareness and research funding.this oversight leaves vulnerable populations, such as young children, the elderly, and those with weakened immune systems, at greater risk.Raising awareness and prioritizing research are essential steps in addressing this silent threat.
Conclusion
Human metapneumovirus may not dominate headlines,but its impact on respiratory health is undeniable.As we continue to navigate the challenges posed by emerging viruses, understanding hMPV and investing in preventive measures and research are critical. By fostering greater awareness and collaboration, we can build a more resilient society equipped to tackle this and other health threats.
Dr. Andi Wijayanto SpP, a renowned lung specialist, shares insights on preventing HMPV transmission.
The Role of Neutralizing Antibodies in Combating hMPV
In the ongoing battle against human metapneumovirus (hMPV), neutralizing monoclonal antibodies (nMAbs) have emerged as a beacon of hope. These specialized antibodies are not only pivotal in vaccine development but also serve as powerful therapeutic tools in managing infectious diseases.Recent research underscores their importance, stating, “neutralising monoclonal antibodies are the core effectors of vaccines and are essential therapeutic immune drugs against infectious diseases.”
Though, progress in developing nMAbs for hMPV has been sluggish, highlighting a critical need for increased investment and research. Bridging the gap between scientific breakthroughs and real-world applications remains a pressing challenge.
Prevention Strategies: what You Need to Know
Dr. Andi Wijayanto SpP, a leading authority in respiratory health, stresses the significance of preventive measures to curb hMPV transmission. While a vaccine is still in development, adopting simple yet effective practices can make a significant difference. Key strategies include:
- Maintaining rigorous hand hygiene, particularly during peak flu seasons.
- Limiting close contact with individuals exhibiting symptoms of respiratory infections.
- Ensuring proper ventilation in indoor environments to reduce airborne transmission risks.
Why hMPV Deserves more Attention
Despite its significant impact on public health,human metapneumovirus frequently enough remains overshadowed by more prominent respiratory viruses. The absence of targeted treatments and vaccines underscores the urgent need for heightened research and innovation in this field.
As Dr. Wijayanto aptly notes, “Prevention is our strongest weapon in the fight against hMPV.” This sentiment resonates deeply, especially when considering the virus’s potential to cause severe respiratory infections, particularly in vulnerable populations.
By prioritizing research, funding, and public awareness, we can better equip ourselves to tackle hMPV and safeguard global health. The journey ahead might potentially be challenging, but with concerted efforts, meaningful progress is within reach.
Understanding Human Metapneumovirus (HMPV): Symptoms, Prevention, and Global Impact
Human Metapneumovirus (HMPV) is a respiratory virus that has been gaining attention due to its increasing prevalence worldwide. This virus, which primarily affects vulnerable groups such as young children, elderly adults, and individuals with weakened immune systems, has been linked to significant outbreaks in regions like China, Malaysia, and Hong Kong. With cases on the rise globally, understanding HMPV and how to protect yourself has never been more critical.
What is Human Metapneumovirus (HMPV)?
HMPV is a respiratory virus that often goes unnoticed but can have serious health implications. Similar to the common cold and flu, it can cause symptoms ranging from mild coughs and congestion to severe respiratory distress, particularly in high-risk individuals. Despite its low profile, recent data underscores its growing role in global health challenges.
Who is Most at Risk?
Certain groups are more vulnerable to severe HMPV infections. these include:
- Young children, whose immune systems are still developing.
- Elderly adults, especially those with pre-existing health conditions.
- Individuals with weakened immune systems, such as those undergoing chemotherapy or living with chronic illnesses.
For these populations, HMPV can lead to complications like pneumonia or bronchitis, making early detection and prevention essential.
How to Protect Yourself and Others
Preventing HMPV involves adopting habits that reduce the risk of respiratory infections. A pulmonary specialist emphasized the importance of maintaining good air circulation by opening windows or using air filters. Additionally, he highlighted the need for frequent handwashing, maintaining physical distance, and wearing masks when feeling unwell.
“Avoid touching your face and sharing food or eating utensils,” he added,underscoring the simple yet effective measures that can curb the spread of the virus.
raising Awareness About HMPV
public education plays a vital role in combating HMPV. As one expert noted, “it is indeed hoped that the education provided today will help the public be more aware of the risk of HMPV infection and other respiratory diseases.” By staying informed and taking proactive steps, individuals can protect themselves and their communities.
Conclusion
Human Metapneumovirus may not be as widely recognized as other respiratory viruses, but its impact is undeniable. With rising cases globally, understanding its symptoms, risks, and prevention strategies is essential. By prioritizing good hygiene, maintaining clean air, and supporting public health initiatives, we can mitigate the spread of HMPV and protect those most at risk.
Understanding HMPV: A Silent Threat to Respiratory Health
Human Metapneumovirus (HMPV) emerged as a significant discovery in 2001 when Dutch researchers, including Bernadette van den Hoogen and G.J. Dureen, identified it as a distinct respiratory virus. Despite its discovery over two decades ago, HMPV remains underrecognized, often overshadowed by more familiar viruses like influenza and RSV. Compounding the issue is the lack of a specific treatment or vaccine, leaving healthcare providers with limited tools to combat its spread.
Dr. Ahmad Ridhoi MSi explained the structure and mechanism of the HMPV virus during the ITS Medics webinar on Wednesday (15/1).
HMPV is a stealthy respiratory virus that frequently enough flies under the radar due to its nonspecific symptoms, which can easily be mistaken for a common cold. However, for vulnerable groups such as infants, the elderly, and those with weakened immune systems, HMPV can escalate into severe respiratory conditions like pneumonia and bronchitis.This makes it a pressing public health concern,particularly during peak respiratory virus seasons.
The Discovery and Unique Traits of HMPV
The identification of HMPV was a groundbreaking moment in virology. Before its discovery, many respiratory infections were incorrectly attributed to other viruses, such as influenza or respiratory syncytial virus (RSV). HMPV’s unique genetic structure and behaviour set it apart, revealing a new player in the landscape of respiratory illnesses. Its ability to evade detection and mimic other viruses has made it a challenging adversary for both clinicians and researchers.
Why HMPV Continues to Challenge Public Health
HMPV’s persistence as a public health threat stems from several factors. its nonspecific symptoms make it challenging to diagnose without specialized testing, which is not always readily available. Additionally, the lack of targeted treatments or vaccines leaves healthcare providers reliant on supportive care to manage symptoms. This is particularly concerning for high-risk populations, where the virus can lead to severe complications and even hospitalization.
Dr. Ahmad Ridhoi msi, during the ITS Medics webinar, emphasized the importance of understanding the virus’s structure and mechanisms. “By unraveling how HMPV operates, we can develop better strategies to detect, prevent, and ultimately treat this elusive virus,” he stated.
Prevention and Awareness: The Path Forward
While HMPV poses significant challenges, there are steps individuals and communities can take to reduce its impact. Practicing good hygiene, such as frequent handwashing and covering coughs, can definitely help limit the spread of respiratory viruses. Improving indoor air quality and staying informed about the latest research are also crucial.Public awareness campaigns can play a vital role in educating people about the risks of HMPV and the importance of early detection.
As research continues, the hope is that new treatments and preventive measures will emerge. Until than, understanding HMPV and its effects on respiratory health remains a critical step in safeguarding vulnerable populations and reducing the overall burden of this often-overlooked virus.
Understanding Human Metapneumovirus (HMPV): A Persistent respiratory Threat
Respiratory infections have long been a global health concern, with viruses like influenza and RSV often taking the spotlight.However, another lesser-known but equally significant pathogen, Human metapneumovirus (HMPV), has been quietly contributing to the burden of respiratory illnesses. discovered in 2001, HMPV has since been recognized as a key player in respiratory infections, particularly among children, the elderly, and immunocompromised individuals.
What Is HMPV?
HMPV belongs to the Paramyxoviridae family, a group that includes other notorious respiratory viruses. Despite its genetic similarities to its relatives, HMPV stands out due to its unique replication mechanisms and clinical manifestations. Dr. Ahmad Ridhoi MSi, a virology expert, explained during the ITS Medics webinar, “HMPV’s distinct genetic structure and behavior make it a challenging virus to study and combat.”
Why HMPV Remains a Challenge
More than two decades after its discovery,HMPV continues to pose a significant public health challenge. One of the primary obstacles is the lack of targeted antiviral therapies and vaccines. Unlike RSV and influenza, which have specific treatments and preventive measures, HMPV remains largely unaddressed in the medical arsenal.
Dr. Ridhoi emphasized this gap during the webinar,stating,”The absence of a cure for HMPV underscores the need for continued research and advancement in this area.Until we have effective treatments, prevention remains our best strategy.”
the Importance of Awareness and prevention
In the absence of a cure, raising awareness about HMPV and implementing preventive measures are critical. Simple yet effective steps, such as practicing good hand hygiene, avoiding close contact with infected individuals, and covering coughs and sneezes, can significantly reduce the spread of the virus.
Public health campaigns and educational initiatives,like the ITS Medics webinar,play a vital role in spreading knowledge about HMPV and other emerging health threats. By fostering a deeper understanding of the virus and its transmission, individuals and communities can take proactive steps to protect themselves.
Conclusion
Human metapneumovirus, though discovered over two decades ago, remains a significant yet underrecognized cause of respiratory infections.The lack of targeted treatments highlights the urgent need for continued research and public health efforts. As Dr. Ridhoi aptly noted, “Awareness and prevention are our most effective tools in the fight against HMPV.” By staying informed and adopting preventive measures, we can collectively mitigate the impact of this persistent respiratory threat.
What are the primary symptoms of HMPV infection?
Ry illnesses worldwide.First identified in 2001, HMPV has as been recognized as a major cause of respiratory infections, particularly in vulnerable populations such as young children, the elderly, and immunocompromised individuals. Despite its impact,HMPV remains underdiagnosed and underreported,often overshadowed by more familiar respiratory viruses. This article delves into the characteristics of HMPV, its clinical importance, and the ongoing efforts to better understand and combat this persistent respiratory threat.
What is Human Metapneumovirus (HMPV)?
HMPV is a single-stranded RNA virus belonging to the Pneumoviridae family, closely related to respiratory syncytial virus (RSV). It was first discovered in the Netherlands by researchers who identified it as a previously unknown cause of respiratory infections in children. Since then, HMPV has been found to circulate globally, with seasonal peaks typically occurring in late winter and early spring, overlapping with influenza and RSV seasons.
HMPV primarily affects the upper and lower respiratory tract,causing symptoms ranging from mild cold-like illness to severe lower respiratory tract infections (LRTIs) such as pneumonia and bronchiolitis. In healthy individuals,HMPV infections are often self-limiting,but in high-risk groups,the virus can lead to hospitalization and,in rare cases,death.
Clinical Presentation and Diagnosis
The symptoms of HMPV infection are nonspecific and can easily be mistaken for those caused by other respiratory viruses.Common symptoms include:
- Cough
- Nasal congestion
- Fever
- Sore throat
- Shortness of breath (in severe cases)
In severe infections, particularly in vulnerable populations, HMPV can progress to pneumonia, bronchiolitis, or exacerbations of chronic lung diseases such as asthma or chronic obstructive pulmonary disease (COPD).
Diagnosing HMPV can be challenging due to its nonspecific presentation and the lack of routine testing in many healthcare settings. Molecular diagnostic tests, such as reverse transcription-polymerase chain reaction (RT-PCR), are the gold standard for detecting HMPV.Though, these tests are not always widely available, leading to underdiagnosis and underestimation of the virusS true burden.
Who is Most at Risk?
Certain groups are more susceptible to severe HMPV infections:
- Young Children: Infants and toddlers, especially those under the age of 2, are at higher risk due to their immature immune systems.
- Elderly Adults: older adults, particularly those with underlying health conditions, are more likely to experience severe complications.
- Immunocompromised Individuals: People with weakened immune systems, such as those undergoing chemotherapy or living with HIV, are at increased risk of severe disease.
- Individuals with Chronic Respiratory Conditions: Those with asthma, COPD, or other chronic lung diseases are more likely to experience exacerbations triggered by HMPV.
Why is HMPV a Growing Concern?
Several factors contribute to the growing recognition of HMPV as a significant public health threat:
- Underdiagnosis: The lack of routine testing means many cases go undetected, leading to an underestimation of its prevalence and impact.
- Overlap with Other Viruses: HMPV often circulates alongside influenza and RSV, making it challenging to distinguish its contribution to respiratory illness outbreaks.
- Lack of Specific Treatments: There are currently no antiviral therapies specifically approved for HMPV. Treatment is primarily supportive, focusing on symptom management.
- No Vaccine: Unlike influenza and RSV, there is no vaccine available to prevent HMPV infections, leaving vulnerable populations unprotected.
Prevention and Control Measures
While there is no specific treatment or vaccine for HMPV,several preventive measures can help reduce the risk of infection:
- Hand Hygiene: Frequent handwashing with soap and water or using alcohol-based hand sanitizers can help prevent the spread of respiratory viruses.
- Respiratory Etiquette: Covering coughs and sneezes with a tissue or elbow can reduce the transmission of respiratory droplets.
- Avoiding Close Contact: Staying away from individuals who are sick and avoiding crowded places during peak respiratory virus seasons can lower the risk of infection.
- Improving Indoor Air Quality: Ensuring proper ventilation and using air purifiers can help reduce the concentration of airborne viruses.
- Public Awareness: Educating the public about HMPV and its risks can encourage proactive measures to prevent its spread.
The Road Ahead: Research and Development
Efforts to better understand and combat HMPV are ongoing. Researchers are working to:
- Develop rapid and accurate diagnostic tools for widespread use.
- Investigate potential antiviral therapies to treat HMPV infections.
- Explore vaccine candidates to provide immunity against the virus.
- Study the virus’s epidemiology and genetic diversity to inform public health strategies.
As Dr. Ahmad Ridhoi MSi highlighted during the ITS Medics webinar, understanding the virus’s structure and mechanisms is crucial for developing effective interventions. “By unraveling how HMPV operates, we can develop better strategies to detect, prevent, and ultimately treat this elusive virus,” he stated.
Conclusion
Human Metapneumovirus (HMPV) may not be as well-known as other respiratory viruses, but its impact on global health is significant. With rising cases and no specific treatments or vaccines available, HMPV poses a persistent challenge, particularly for vulnerable populations. By raising awareness, improving diagnostic capabilities, and investing in research, we can better understand and mitigate the effects of this frequently enough-overlooked virus. in the meantime, adopting preventive measures and supporting public health initiatives remain our best defense against HMPV and other respiratory threats.



