The sociodemographic and obstetric characteristics of the extensive study population, as well as the subgroups categorized by hemoglobin (Hb) ranges, are comprehensively outlined in Table 1. The study examined a staggering 454,815 pregnant women, revealing an average age of 29.2 years, with a standard deviation of 4.3 years. Remarkably, the median gestational age at which the Hb testing took place was determined to be 10.6 weeks, with an interquartile range (IQR) of 8.6 to 12.2 weeks. Within this population, a striking 96.9% identified as Han ethnicity, while only 1.0% were Tibetans, and 2.1% represented various other ethnic minorities from a diversity of 53 ethnic groups. A significant 70.9% of the participants held a rural hukou status; furthermore, 67.1% reported a prepregnancy body mass index (BMI) falling within the range of 18.5 to 23.9 kg/m². Additionally, nearly half of the women, at 47.7%, had achieved a college or university-level education. Importantly, more than half of the females surveyed were nulliparous; a small fraction, specifically 1.8%, conceived through in vitro fertilization, while 1.1% experienced multiple pregnancies. Notably, women who exhibited higher Hb concentrations during the first trimester were generally younger, nulliparous, of Han ethnicity, employed, and showcased urban hukou status, alongside having achieved higher education levels and maintained higher prepregnancy BMIs. In contrast, women with lower Hb concentrations tended to exhibit the opposite characteristics.
Table 1 Sociodemographic and obstetric characteristics of the study population and subgroups stratified by hemoglobin ranges in the first trimester in Chengdu, 2019–2023
Within this research, the average Hb concentration was gauged at approximately 10.3 weeks of gestation. Among the impressive cohort of 454,815 pregnant women, the mean Hb concentration observed in the first trimester recorded at 126.0 g/L, showcasing a standard deviation of 10.5 g/L. Alarmingly, a total of 26,390 females, which accounts for 5.8%, were found to have anemia, disaggregated into categories with 20,105 individuals (4.4%) experiencing mild anemia (Hb level between 100 and 109 g/L), 6,232 (1.4%) suffering from moderate anemia (Hb level between 70 and 99 g/L), and a mere 53 (0.01%) presenting with severe anemia (Hb level < 70 g/L). The anticipated risk of anemia during early pregnancy demonstrated a decline from 8.0% (95% Confidence Interval [CI]: 7.2–8.8%) at the age of 15 years to 5.2% (95% CI: 5.1–5.3%) at the age of 26 years, before surging to 8.8% (95% CI: 7.8–9.9%) by the age of 49 years.
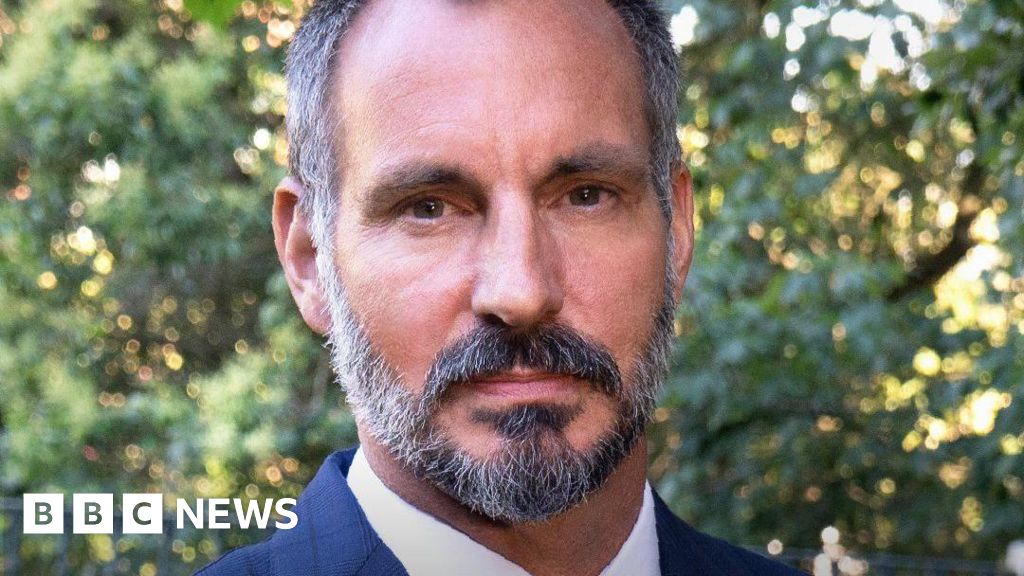
Fig. 2
Estimated absolute risk of anemia in the first trimester by maternal age
Table 2 provides an analytical overview of the prevalence of adverse pregnancy outcomes. Intriguingly, the observed percentages of pregnant women who subsequently developed gestational diabetes mellitus (GDM) and gestational hypertensive disorders (GHD) showed an upward trend corresponding to increasing Hb concentrations during the first trimester. Particularly, in the Hb ≥ 140 g/L category, a notable 21.3% and 9.7% of participants were diagnosed with GDM and GHD, respectively, significantly surpassing the corresponding incidences of 13.4% for GDM and 5.1% for GHD within the moderate-severe anemia group (Hb ≤ 99 g/L). Furthermore, approximately half of the women within the Hb 110–119 g/L cohort underwent cesarean sections, a rate which was comparatively lower than in other Hb categories. Conversely, the rates of preterm birth (PTB), low birth weight (LBW), and small for gestational age (SGA) were least prevalent in the Hb 120–129 g/L category, with higher rates recorded in both the high and low Hb concentration groups. Although the instances of stillbirth and Apgar scores remained statistically insignificant, showing a p-value greater than 0.05, the implications are noteworthy.
Table 2 Adverse pregnancy outcomes by hemoglobin concentrations in the first trimester in Chengdu, 2019–2023
The findings derived from the multivariable logistic regression models, as delineated in Table 3, evaluated the relationships between Hb concentrations during the first trimester and the subsequent odds of adverse pregnancy outcomes. For this analysis, the Hb concentration within the 110–119 g/L category served as the reference point. The models accounted for a variety of possible confounders, such as year, maternal age, ethnicity, education level, parity, prepregnancy BMI, and the occurrence of multiple pregnancies. A comparison of adjusted odds ratios (aORs) across different Hb concentration categories revealed a notably elevated risk for GDM and GHD in line with increasing Hb levels. Specifically, when compared to the reference group with Hb concentrations of 110–119 g/L, those classified with Hb concentrations ≥ 140 g/L and ≤ 99 g/L exhibited significant increases in the odds of PTB (aOR: 1.20, 95% CI: 1.13, 1.26 for Hb ≥ 140 g/L; aOR: 1.15, 95% CI: 1.03, 1.29 for Hb ≤ 99 g/L). Similarly, for adverse outcomes associated with cesarean delivery, LBW, and SGA, the highest risk factors were identified within groups exhibiting Hb ≤ 99 g/L (aOR: 1.15, 95% CI: 1.09, 1.22 for cesarean delivery; aOR: 1.40, 95% CI: 1.24, 1.58 for LBW; aOR: 1.43, 95% CI: 1.31, 1.57 for SGA) and Hb ≥ 140 g/L (aOR: 1.11, 95% CI: 1.08, 1.14 for cesarean delivery; aOR: 1.25, 95% CI: 1.17, 1.33 for LBW; aOR: 1.09, 95% CI: 1.04, 1.15 for SGA), in comparison to the 110–119 g/L reference range. Furthermore, exploratory logistic regression employing restricted cubic spline models indicated a U-shaped relationship between continuous Hb concentrations and their adjusted odds ratios for PTB, cesarean delivery, LBW, and SGA, with statistical significance (p < 0.05).
Table 3 The associations of hemoglobin concentrations in the first trimester with the odds of adverse pregnancy outcomes in Chengdu, 2019–2023
Results from stratified analyses, as detailed in Supplemental Tables 1 to 4, revealed consistent associations regarding singleton pregnancies and their corresponding adverse outcomes. Interestingly, in cases of multiple pregnancies, a positive correlation persisted between the first trimester Hb concentrations and their odds ratios for GDM and GHD. Nonetheless, there appeared to be minimal associations between Hb concentrations during the first trimester and the likelihood of cesarean delivery, LBW, and SGA, even after controlling for potential confounding variables, with p-values exceeding 0.05.
How can healthcare providers improve screening and management of hemoglobin levels in pregnant women based on Dr. Zhao’s findings?
**Interview with Dr. Lin Zhao, Lead Researcher on the Study of Hemoglobin Levels in Pregnant Women in Chengdu**
**Editor:** Thank you for joining us, Dr. Zhao. Your recent study has provided remarkable insights into the hemoglobin levels in a large population of pregnant women. Can you tell us a little about the main findings?
**Dr. Zhao:** Thank you for having me. Our study examined over 454,000 pregnant women in Chengdu and found an average hemoglobin concentration of 126.0 g/L in the first trimester. Notably, we discovered that about 5.8% of participants were anemic, with varying degrees of severity. It’s concerning because anemia can have serious implications for both maternal and fetal health.
**Editor:** That’s quite a significant number. Could you elaborate on the sociodemographic characteristics of the study population?
**Dr. Zhao:** Certainly. The majority of the participants, 96.9%, identified as Han ethnicity, with 70.9% holding rural hukou status. Our findings also indicated that nearly half of the women had a college degree or higher, and a significant portion were nulliparous. It’s interesting to note that those with higher hemoglobin concentrations tended to be younger, urban, and had higher education and BMI levels.
**Editor:** Such sociodemographic factors can indeed influence health outcomes. What did your findings reveal about the relationship between hemoglobin concentrations and adverse pregnancy outcomes?
**Dr. Zhao:** Our research highlighted a concerning trend: as hemoglobin levels increased, so did the rates of gestational diabetes mellitus and gestational hypertensive disorders. For instance, in women with hemoglobin levels of 140 g/L or higher, 21.3% developed gestational diabetes, compared to just 13.4% in those with moderate to severe anemia. This suggests that both high and low hemoglobin levels can pose risks during pregnancy.
**Editor:** That’s quite intriguing—was there a particular hemoglobin range that appeared to have the best outcomes?
**Dr. Zhao:** Yes, the group with hemoglobin concentrations between 120–129 g/L exhibited the lowest rates of preterm birth, low birth weight, and small for gestational age infants. It seems there may be an optimal range where pregnancy outcomes are more favorable.
**Editor:** What do you hope will come from this study? Are there any implications for clinical practice?
**Dr. Zhao:** We hope our findings will lead to improved screening and management of hemoglobin levels in pregnant women. It’s vital for healthcare providers to understand the risks associated with both low and high hemoglobin concentrations and to tailor care accordingly. Education and awareness among expectant mothers about nutrition and health during pregnancy are also crucial.
**Editor:** Thank you, Dr. Zhao, for sharing your important research with us. Your findings will surely contribute to better health outcomes for pregnant women.
**Dr. Zhao:** Thank you for the opportunity to discuss our work. I hope it raises awareness and prompts further research in this critical area.