- Martha Henriques
- BBC Future
3 hours ago
image source,SPL
Oral health affects far beyond the mouth, affecting everything from the brain to the heart.
Teeth and gums have a wide range of effects on your health and are linked to Alzheimer’s disease, diabetes and cardiovascular disease.
Crowded teeth, misaligned teeth, cavities and inflamed gums are well known problems with teeth. What makes modern humans unique is that painstaking intervention is required every day to keep our teeth and gums from getting sick.
Oral health is not limited to toothaches and sore gums, it affects everything from our diet to our overall health and can even lead to our risk of death.
This is because oral disease is not always confined to the mouth. The strong link between oral health and some of the world’s worst diseases, including cardiovascular disease, diabetes and Alzheimer’s disease, is emerging, showing that the mouth is like a mirror of physical health and disease, and is the whole of our lives An indicator of happiness.
Unfortunately, oral health is most often overlooked. Periodontitis, or deep gum disease, is the second most common oral disease following dental caries, affecting more than 47% of adults over the age of 30. Among people over the age of 65, 64% had moderate or severe periodontitis. Globally, it is the 11th most common disease in the world.
Periodontitis is an infection that is not a symptom on the surface of your gums that you can see when you smile, but deep down. During the initial stages of inflammation of the gum surface (gingivitis), bacteria travel along the gum line into the root pockets, where they erode the structures that support the teeth. Due to the insidious nature of periodontitis, many patients with periodontitis do not realize it until the disease has advanced to an advanced stage. The disease has a genetic component and is also influenced by oral hygiene.
For most people, the disease doesn’t become apparent until they are in their 40s or 50s, said Sim K Singhrao, a senior research fellow at the University of Central Lancashire’s School of Dentistry. By this time, severe damage may have disrupted the structure of the tooth and there is a risk of tooth loss. In fact, the infection had been spreading bacteria, such as Treponema pallidum and Porphyromonas gingivalis, in the bloodstream for decades.
It is this disease-causing bacteria that lives in the gums and blood for a long time and affects health beyond the mouth.

image source,Getty Images
Part of the danger of periodontitis is that many patients don’t appreciate it because it is often asymptomatic.
“If you think of blood as a bus, it carries passengers — like bacteria in the mouth — all over the body… some will be in the brain, some will be in the arteries, some will be in the arteries, some will be in the arteries, some will be in the arteries, in the pancreas or liver.”
When these organs become weakened, these bacteria can cause inflammation and initiate or exacerbate other inflammatory diseases.
In fact, periodontitis is associated with some of the most prevalent non-communicable diseases in the world: cardiovascular disease, diabetes, Alzheimer’s disease, obesity, various cancers, rheumatoid arthritis, Parkinson’s disease, pneumonia and pregnancy complication.
In many cases, this is a two-way relationship. For example, periodontitis can aggravate atherosclerosis, arterial wall sclerosis, etc., and the presence of atherosclerosis can easily make patients suffer from periodontitis. There are currently no randomized controlled trials (RCTs) considered the gold standard of medical investigation to delve into this relationship; ethically, these trials are difficult to conduct because a group of people with periodontitis is required over an extended period of time No treatment was given to observe its effect on atherosclerosis. However, periodontitis-causing bacteria normally found only in the mouth were found embedded in atherosclerotic plaques.
Of all these chronic diseases, the bidirectional link between diabetes and periodontitis was the strongest. People with type 2 diabetes are three times more likely to develop periodontitis than people without periodontitis. For people with type 2 diabetes and periodontitis, infections can worsen their body’s inability to control blood sugar levels.
but. What is the reason behind this connection?

image source,Getty Images
Periodontitis has a genetic component, but the risk of developing periodontitis can be minimized through careful oral hygiene.
This occurs as bacteria travel from deep within the gums into the bloodstream. When the immune system detects bacteria or other pathogens, immune cells release a flood of cell-messaging molecules called inflammatory markers. Cell signaling molecules for these inflammatory markers. These inflammatory markers help the immune system attack and kill invading pathogens. The redness that appears around the wound is the result of an inflammatory reaction.
In the short term, inflammatory markers can serve as a good guide for the immune system to target sites of possible infection. But when these sentinels linger in the body, a whole host of problems arise.
Most diseases associated with periodontitis have a recognized inflammatory factor. For example, nearly 30 years ago, an inflammatory marker called tumor necrosis factor-alpha was found to increase insulin resistance in people with diabetes. Soon following, a slew of other markers of inflammation were found to exacerbate obesity and type 2 diabetes. This dense network of inflammatory markers has triggered research aimed at treating diabetes by inhibiting chronic inflammation.
Continued intrusion of bacteria from an infection lurking in the gums does just the opposite.
“All inflammatory diseases are interconnected and affect each other,” said Palle Holmstrup, emeritus professor at the Department of Dentistry at the University of Copenhagen.
“Periodontitis is one of the most common inflammatory diseases in the human body, maybe even the most common.
“This is the same inflammatory mediator that is active in multiple inflammatory diseases (rheumatoid arthritis, heart disease, diabetes, etc.). If you have periodontitis, you have increased low-grade inflammation throughout your body.”
In humans, it is difficult to directly study how treating periodontitis can alleviate diseases such as diabetes, for the same ethical reasons as treating atherosclerosis: you cannot deny treating a patient’s disease for the sake of research, especially if you suspect that it may aggravate their other diseases. This makes it especially difficult to study this complex, interconnected inflammatory disease, and to pinpoint cause and effect.
However, Holmtruk’s team has already measured the effects of periodontitis on diabetes in rats. His group looked at the difference in blood sugar responses in diabetic rats with periodontitis and those without. Periodontitis causes a 30% increase in postprandial blood sugar.
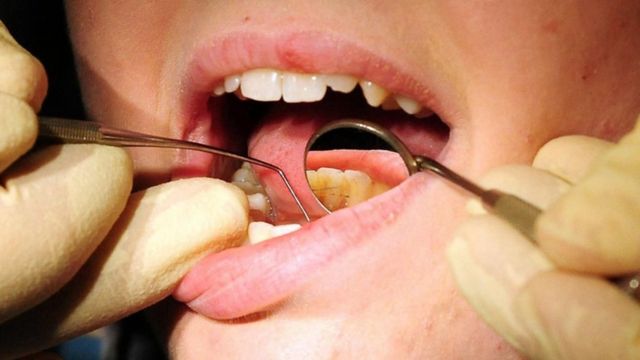
image source,PA / Rui Vieira
If not careful, periodontitis can lead to tooth loss, as well as health risks.
If periodontitis is aggressive and left untreated, it can eventually lead to tooth loss. In addition to decades of chronic inflammation, tooth loss brings a host of new health risks, including cognitive decline and dementia.
Bei Wu, dean and professor of global health at New York University’s Rory Meyers College of Nursing, has found an association: The more teeth you lose, the risk of cognitive decline and dementia the bigger. In the largest study of its kind, Wu looked at the health data of 34,000 patients in the United States and found that for every tooth a person lost, their risk of cognitive impairment and dementia increased by 1.4%. An increase of 1.1%.
Overall, those who lost their teeth had a 48 percent increased risk of cognitive impairment and a 28 percent increased risk of dementia compared with those with intact teeth.
Tooth loss is a risk factor for dementia that has been largely ignored. Wu said she is usually surprised when she points out the relationship between the two. “Oral health is the missing piece,” Wu said. “We’re trying to provide evidence that it should be an important part of good health.”
While periodontitis may be a common cause of tooth loss, there may be other causes besides inflammation. Wu’s tooth loss research so far has only investigated correlation, not causation, but she wants to investigate the role of nutrition in this relationship, among other factors.
“A good denture can improve nutrient intake and also improve your ability to chew,” Wu said. “This might increase blood flow, which might have an impact on cognitive function — but that’s still just a hypothesis.”

image source,SPL
Every time we brush our teeth, we have an opportunity to improve our broader health.
The link between oral health and other diseases has a very important consequence: reducing the risk of periodontitis is easy, and if you already have periodontitis, it can be effectively treated.
“If we brush our teeth properly and maintain good oral hygiene, it is possible to prevent periodontitis from developing,” Professor Wu said.
If dental disease does occur, it can be treated in the early stages with scaling and root planing, which will scrape away the microbes below the gum line. If you have severe periodontitis, the solution may include surgery, “which means you loosen the soft tissue of the gum, clean the surface of the root, and then put the tissue back in,” says Holmsch.
The problem is testing, as the disease is often asymptomatic, coupled with the common misconception that unless you have a severe toothache, you don’t need to go to the dentist. The solution is also simple: you need to see your dentist regularly, without delay.



