2024-11-01 07:24:00
Being overweight in midlife has been linked to greater risk of developing Alzheimer’s disease or dementia, and a new study shows that brain changes in obese people mirror some of those with Alzheimer’s.
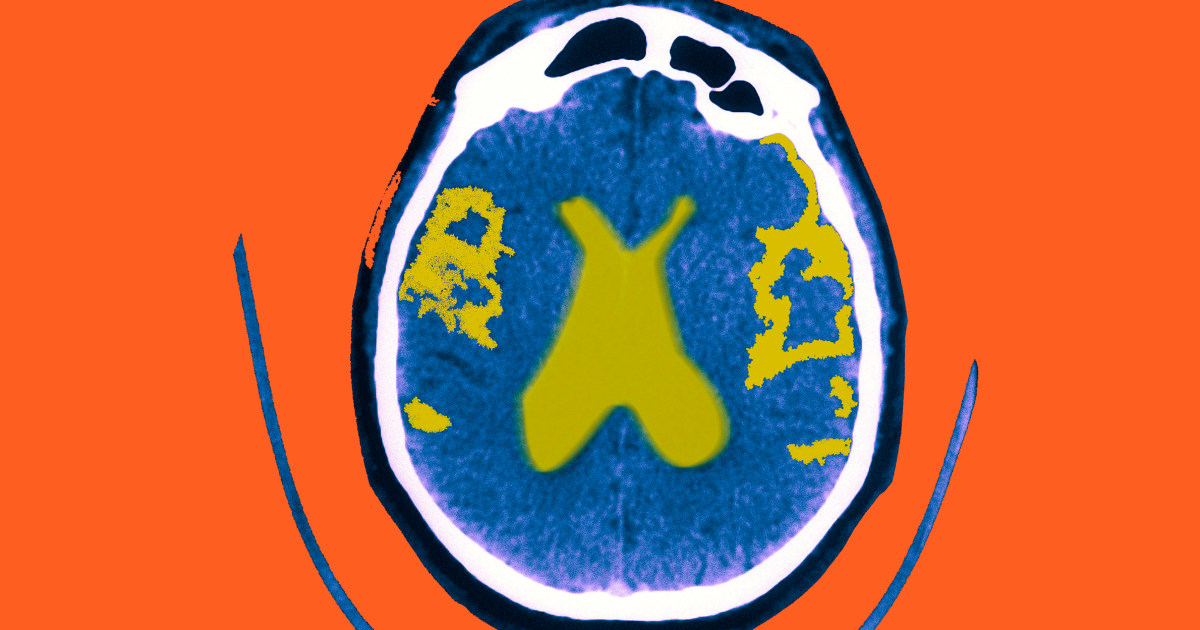
Scientists at McGill University in Montreal analyzed brain scans of more than 1,300 people in the first research to directly compare the patterns of brain shrinkage in obese people and in Alzheimer’s patients.
The scans revealed similar brain thinning in regions involved in learning, memory and judgment in both groups, according to the report published Tuesday in the Journal of Alzheimer’s Disease.
Obesity can cause changes in the body that are associated with raising the risk of Alzheimer’s, including damage to the brain’s blood vessels and the accumulation of abnormal proteins, earlier studies have found. The new research takes it a step further.
“We showed that there is a similarity between the brains of people who are obese and those with Alzheimer’s,” said the study’s first author, Filip Morys, a postdoctoral neuroscience researcher at McGill University. “And it boils down to the thickness of the cerebral cortex.”
The cerebral cortex, which in humans is responsible for higher brain functions such as speech, perception, long-term memory and judgment, is the outer layer of the brain.
Thinning in that brain region might reflect a decrease in the number of brain cells, Morys said.
The McGill researchers suspect that obese people, and possibly those who are overweight — a BMI of 25 to 25.9 — might be able to slow cognitive decline if they can get closer to a healthy weight.
Morys wasn’t able to identify a target weight.
Latest stories on weight loss
Why is obesity hazardous to the brain?
The science isn’t clear. Other conditions that are bad for the brain — including high blood pressure, high cholesterol and type 2 diabetes — are also connected to obesity, Morys notes.
To take a closer look at the impact of obesity on brain structure, Morys and his colleagues scrutinized brain scans from 341 Alzheimer’s patients and 341 obese individuals with a BMI of 30 or more, along with scans from 682 healthy individuals.
All of the brain scans and other information came from two large health databases: the U.K. Biobank and the Alzheimer’s Disease Neuroimaging Initiative, a program that recruits participants across North America and is funded in part by the National Institutes of Health.
Cognitive tests taken by the obese individuals in the study did not reveal obvious mental deficits, but it’s possible that subtle changes in cognition related to the thinning seen on the brain scans might not be picked up on the types of tests used to evaluate mental status, Morys said.
The new research “showed us something we didn’t know before,” said metabolism researcher Sabrina Diano, director of the Institute of Human Nutrition at the Columbia Irving Medical Center.
“The study showed that obese individuals and those with Alzheimer’s disease have common areas of the brain that are smaller in size, possibly due to a neurodegenerative process,” meaning that the nerve cells in these regions may be experiencing damage and could be dying, Diano said.
The scans can’t show that obesity is causing the thinning of these areas, but it makes sense that controlling body weight might be a way to reduce the risks, she said.
“We know that if you take a mouse that has a genetic predisposition to develop Alzheimer’s and you put that mouse on a diet rich in carbohydrates and fat —similar to the Western diet — you can induce increases in body weight in the animal and as they gain weight cognitive impairment and the brain degeneration is accelerated,” Diano said.
Could weight loss reverse the damage?
The study opens the door to further exploration of whether weight loss might reverse some of the brain changes, said Dr. Joseph Malone, an assistant professor of neurology in the cognitive disorders division at the University of Pittsburgh. Malone was not involved with the study.
“We do know that obesity is associated with other diseases that can affect the blood vessels in the brain, such as type 2 diabetes, high blood pressure, high cholesterol and inflammation, all of which could lead to the breakdown of blood vessels in the brain and thus contribute to brain cell death,” Malone said.
While the obese individuals in the study did not show memory declines, it’s possible that what the researchers are seeing is an early stage in the development of Alzheimer’s, Malone suggested.
One limitation in the research is that it doesn’t directly report on what people are eating, just that they’re obese, said Linda Van Horn, chief of nutrition at the Northwestern University Feinberg School of Medicine, who was not involved with the study.
“Given that, it leaves a lot of room for speculation and hypothesis generation,” Van Horn said. “Intuitively, you would think it would have an impact on various organs including the brain.”
While the hope is that weight loss could stop or reduce the brain degeneration, “we, unfortunately, are discovering more and more that there are certain points of no return,” Van Horn said.
“I believe, based on examples like osteoporosisthat the chances of reversing the disease are lower than that of preserving what’s there,” she said.
1730523781
#Obesity #brain #similar #Alzheimers #study #suggests
**Interview with Dr. Filip Morys: Understanding the Link Between Midlife Obesity and Cognitive Decline**
**Interviewer:** Thank you for joining us today, Dr. Morys. Your recent research has shed light on the connection between midlife obesity and brain health, particularly in relation to Alzheimer’s disease. Can you summarize your key findings for our listeners?
**Dr. Morys:** Thank you for having me. Our study analyzed brain scans of over 1,300 individuals, comparing those with obesity—defined as a BMI of 30 or more—against patients diagnosed with Alzheimer’s disease. What we found was concerning: similar patterns of brain thinning, particularly in the cerebral cortex, which is crucial for functions like memory and judgment, were observed in both groups. This suggests that obesity may contribute to brain changes akin to those seen in Alzheimer’s.
**Interviewer:** That’s fascinating yet troubling. What do you think are the implications of your findings for midlife individuals who are overweight or obese?
**Dr. Morys:** Our research underscores the importance of maintaining a healthy weight, especially during midlife. We suspect that individuals who are overweight could potentially slow cognitive decline by getting closer to a healthy weight, though the exact target weight is still unclear. While our findings do not confirm that obesity directly causes brain damage, they highlight a likely link that warrants further investigation.
**Interviewer:** You mentioned the cerebral cortex. Can you explain why its thinning is particularly concerning?
**Dr. Morys:** The cerebral cortex is responsible for higher-order functions such as speech, long-term memory, and decision-making. Thinning in this region can be indicative of a reduction in brain cell density, which could signal early neurodegenerative processes. It suggests that responders to cognitive tests may still be experiencing subtle changes that wouldn’t necessarily be evident through standard evaluation methods.
**Interviewer:** Given the risks, what steps do you recommend for those who are worried about the impact of obesity on their brain health?
**Dr. Morys:** While it may not be immediate to reverse any potential damage, adopting a healthier lifestyle can be beneficial. This includes balanced nutrition, regular physical activity, and managing other health factors like blood pressure and cholesterol. These lifestyle changes not only support overall health but may also play a role in mitigating cognitive decline.
**Interviewer:** That sounds like practical advice. Lastly, do you think there’s potential for future studies to explore whether weight loss could reverse some of the brain changes you observed?
**Dr. Morys:** Absolutely. The notion of weight loss reversing some of these changes is an exciting area for future research. Preliminary studies suggest that dietary changes can influence brain health. We hope that ongoing research will clarify these relationships further and provide tangible strategies for individuals concerned with obesity and dementia.
**Interviewer:** Thank you, Dr. Morys, for sharing your insights. It’s a critical issue that affects many, and your work is paving the way for deeper understanding and prevention strategies.
**Dr. Morys:** Thank you for having me. It’s essential we continue the conversation around obesity and brain health.