The Tickle and the Tussle: Why Scratching Itches Seems So Good
Table of Contents
- 1. The Tickle and the Tussle: Why Scratching Itches Seems So Good
- 2. How Scratching Makes skin Inflammation Worse
- 3. The Role of Mast Cells and Nerve Signals
- 4. The Surprising Science of Scratching: When Itching Turns Into an Evolutionary Advantage
- 5. The Surprising Link Between Itch, Inflammation, and Your Immune System
- 6. What causes itching?
- 7. Decoding the Itch: An Interview with Dr.Sarah Hayes
We’ve all been there: an itchy rash that just won’t quit, driving us to scratch until our skin is red and irritated. But why does this feel-good sensation only worsen the problem? A new study published in *science* reveals the surprising science behind this age-old dilemma.
Scratching, that deeply ingrained reflex observed across many species, serves a vital purpose: removing irritants from the skin. Though, in conditions like eczema, where persistent itching is the norm, scratching becomes a vicious cycle.Unlike pain, which compels us to avoid the source, scratching often brings a momentary sense of relief, despite causing further inflammation.
This paradox has long puzzled scientists. Why would an action that clearly harms us feel so satisfying? The study illuminates the intricate chain reaction triggered by scratching. When skin is scratched,pain-sensing neurons release a chemical called substance P. This molecule then activates mast cells, a type of immune cell crucial in allergic reactions.Once activated, mast cells unleash their arsenal: histamines flood the area, intensifying the swelling and inflammation.
Dr. Daniel Kaplan,senior author of the study and a professor of dermatology and immunology at the University of pittsburgh,sheds light on the complex interplay between harm and pleasure. “At first, thes findings seemed to introduce a paradox: If scratching an itch is bad for us, why does it feel so good?” he mused.He continues, “Scratching is often pleasurable, which suggests that, to have evolved, this behavior must provide some kind of benefit. Our study helps resolve this paradox by providing evidence that scratching also provides defense against bacterial skin infections.”
Despite its seemingly self-destructive nature, scratching may offer a vital defense mechanism against harmful bacteria.
Understanding this intricate biological dance between itch,scratch,and inflammation paves the way for more targeted and effective treatment strategies for skin conditions like eczema.
How Scratching Makes skin Inflammation Worse
We all know that scratching an itch can feel good in the moment, but did you know it can actually make skin inflammation worse? New research reveals the surprising link between scratching and increased inflammation, highlighting the complex interplay between our nervous system and immune response.
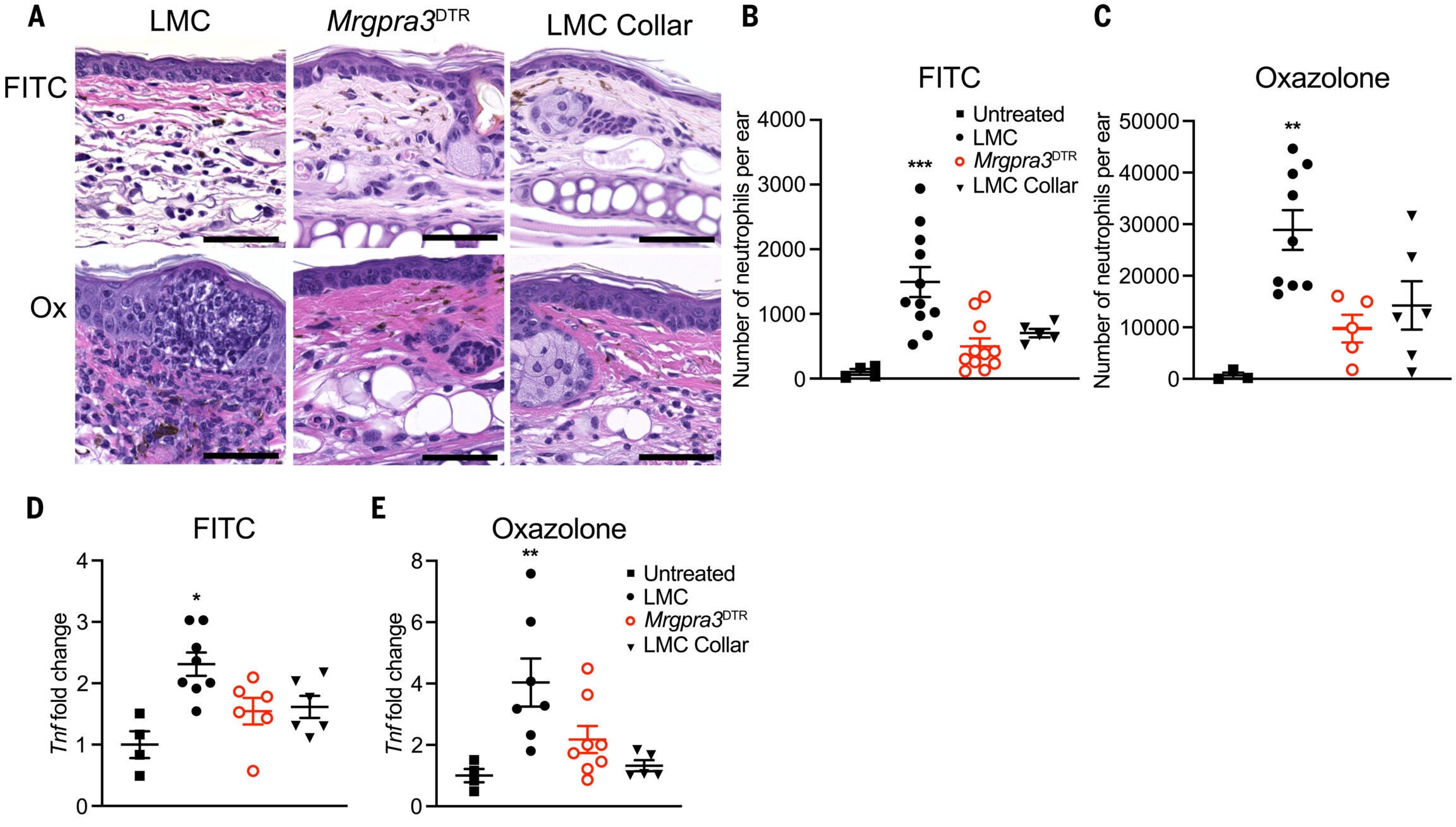
scientists at the University of Pittsburgh conducted experiments on mice to understand how scratching impacts skin inflammation. They induced eczema-like symptoms and observed the inflammatory response in mice with and without the ability to scratch. The results were clear: mice that could scratch experienced substantially more swelling and an influx of neutrophils, immune cells that play a crucial role in inflammation and infection defense.
Interestingly, when mice were prevented from scratching, either by lacking the necessary itch-sensing neuron or by wearing tiny collars to block access to their skin, their inflammation was dramatically reduced. This groundbreaking finding suggests that scratching isn’t simply a reflex response to irritation; it actively fuels the inflammatory process.
Further examination revealed the intricate mechanisms behind this phenomenon. scratching activates pain-sensing neurons, which release a chemical called substance P. Substance P then stimulates mast cells, immune cells known for their role in allergic reactions. Normally, mast cells respond to allergens by triggering mild inflammation and itchiness. However, when scratching enters the equation, mast cells become hyperactivated through a secondary pathway. This dual activation significantly amplifies inflammation, exacerbating conditions like dermatitis.
“In contact dermatitis, mast cells are directly activated by allergens, which drives minor inflammation and itchiness,” explained researcher Kaplan. “In response to scratching, the release of substance P activates mast cells through a second pathway, so the reason that scratching triggers more inflammation in the skin is becuase mast cells have been synergistically activated through two pathways.”
The Role of Mast Cells and Nerve Signals
Mast cells are frequently enough associated with allergic reactions. They release histamines, which increase blood flow and attract immune cells to the affected area.This response helps fight infections but can also contribute to the characteristic redness and swelling associated with allergic responses. This research sheds light on a new dimension of mast cell function, demonstrating their central role in amplifying the inflammatory response triggered by scratching.
Understanding the complex interplay between nerve signals,mast cells,and inflammation opens up new avenues for treating skin conditions like eczema and dermatitis. Perhaps future therapies could target these pathways to reduce the urge to scratch and, in doing so, alleviate the cycle of inflammation and discomfort.
The Surprising Science of Scratching: When Itching Turns Into an Evolutionary Advantage

We all know the feeling: an itch that drives us wild until we relent and scratch. But have you ever wondered why scratching feels so good, even though it often makes the irritation worse in the long run? Research suggests scratching is a complex response, triggering a cascade of reactions in our skin that can have both beneficial and detrimental effects.
Dr. Daniel Kaplan,a dermatologist at the University of Pittsburgh Medical Center,and his team have shed light on the intricate mechanisms behind scratching. According to their research, itching stems from a neuropeptide called substance P interacting with a receptor called MrgprB2 on mast cells, tiny cells found in our skin. When this receptor is activated, mast cells release inflammatory compounds, leading to the redness, swelling, and discomfort we associate with itching.
” Scratching feels relieving in the moment because it interrupts the itch signals being sent to the brain,” explains Dr. Kaplan. “But the scratching itself damages the skin, releasing more inflammatory chemicals, which worsens the symptoms over time.”
Beyond just being a nuisance, itching plays a crucial role in our immune system’s defense against infections. Mast cells, the very cells responsible for the inflammatory response triggered by scratching, also contribute to fighting off bacteria.
Intriguingly, Dr. Kaplan’s team discovered a surprising twist: scratching might actually help combat bacterial infections. In a study using mice, they found that scratching reduced the presence of *Staphylococcus aureus*, a common bacteria responsible for many skin infections.
“.the finding that scratching improves defense against *Staphylococcus aureus* suggests that it could be beneficial in some contexts,” says Dr.Kaplan. “But the damage that scratching does to the skin probably outweighs this benefit when itching is chronic.”
This discovery hints at a possible evolutionary advantage to scratching. Perhaps in our ancestors,the act of scratching,despite its potential for damage,helped to control bacterial infections and promote healing.
The Surprising Link Between Itch, Inflammation, and Your Immune System
We all know the urge to scratch when our skin itches. But did you know that scratching isn’t just a temporary relief; its a complex process that triggers a cascade of events, deeply intertwined with inflammation and your body’s immune response?
Recent groundbreaking research has shed light on this captivating connection. Scientists discovered that scratching activates specific nerve cells called MrgprA3 neurons, which then release chemicals that trigger inflammation.this inflammatory response,while initially intended to protect the skin from harm,can actually worsen the itch and create a vicious cycle.
“Scratching is required for neutrophilic infiltrate and mast cell activation,” explains the research team, highlighting the crucial role scratching plays in this inflammatory process.
This discovery has profound implications for treating skin conditions like eczema, rosacea, and urticaria, which are frequently enough characterized by chronic itching and inflammation.
The research team is now exploring innovative therapies that target these specific pathways, aiming to reduce inflammation without compromising the skin’s essential immune defenses. They are particularly interested in drugs that block receptors involved in mast cell activation, such as MrgprB2, hoping to disrupt the itch-inflammation cycle at its core.
“Blocking specific pathways activated by scratching could prevent the cycle of inflammation while preserving the beneficial effects of immune responses,” explains the research team, offering a glimpse into the future of itch treatment.
While these therapies are still in progress, dermatologists emphasize that managing eczema and other itchy skin conditions requires a multifaceted approach.Moisturizers,anti-inflammatory creams,and avoiding known allergens can help prevent flare-ups. However, understanding the intricate link between itch, inflammation, and the immune system opens exciting new avenues for developing targeted treatments that address the root cause of these persistent skin problems.
We all know the urge to scratch an itchy patch of skin. It feels good in the moment,providing temporary relief. but what if that scratching is actually making your skin condition worse? A recent study sheds light on this seemingly paradoxical relationship, revealing a complex interplay between our instinct to scratch and the inflammatory response.
While scratching might offer a fleeting sense of comfort and even some immune system benefits, researchers now understand that it ultimately fuels inflammation, exacerbating existing skin problems. This discovery overturns long-held assumptions about scratching, paving the way for new treatment strategies.
By delving deeper into the intricate pathways that connect scratching to inflammation, scientists are hopeful that they can develop targeted therapies that address the root cause of chronic skin disorders.
For millions of people battling persistent skin conditions, this research offers a glimmer of hope. Understanding the specific mechanisms behind scratching-induced inflammation could lead to more effective treatments and ultimately improve the quality of life for those suffering from these frequently enough debilitating conditions.
What causes itching?
Decoding the Itch: An Interview with Dr.Sarah Hayes
Archyde News: dr. Hayes, thank you for taking the time to speak with us today. Itching can be incredibly frustrating, especially when it persists for long periods. Can you shed some light on what causes this sensation?
Dr. Sarah Hayes, Dermatologist: It’s my pleasure. You’re right, itching can be incredibly bothersome.It starts with nerve fibers in our skin sensing various irritants, then sending signals to the brain, which interprets them as an itch.
These irritants come in many forms: allergic reactions, dry skin, insect bites, infections, even certain medications can trigger it.
Archyde News: We all know the urge to scratch when we itch. Does scratching actually help, or does it make things worse?
Dr. hayes: It’s a complicated answer.Scratching provides temporary relief because it disrupts the itch signals being sent to the brain. However, scratching also damages the skin, releasing more inflammatory chemicals which usually worsen the inflammation and the itch. It’s kind of a vicious cycle.
Archyde News: So, it sounds like scratching isn’t the best solution. What are some strategies for managing chronic itching that don’t involve scratching?
Dr. hayes: You’re absolutely right. For chronic itching, scratching relief is temporary and often counterproductive. The best approach is multifaceted: • Moisturize yoru skin regularly to soothe dryness.
- Use anti-itch creams or lotions containing hydrocortisone or menthol to reduce inflammation.
- Avoid known triggers, like certain fabrics, soap ingredients, or foods if you have allergies.
- Consider cool compresses or oatmeal baths to soothe irritated skin.
- Talk to your doctor about other treatments like prescription medications or therapies if over-the-counter options aren’t effective.
Archyde News: What about the role of inflammation in itching? It seems like there’s a strong connection there.
Dr. Hayes: You’re spot on. Inflammation plays a critical role in itching. When your skin is irritated, it releases inflammatory chemicals that sensitize nerve fibers, making them more responsive to itch triggers. So, reducing inflammation is key to managing itching.
Archyde News: This has been incredibly informative, Dr. Hayes. For our readers who struggle with chronic itching, what’s your final piece of advice?
Dr. Hayes: Don’t hesitate to seek help from a dermatologist or your primary care physician. They can help you identify the underlying cause of your itching and recommend the best treatment plan for you. Remember, chronic itching isn’t something you have to live with. Help is available.