Ohio State Researchers Uncover New Pathway in Neurodegeneration Linked to FTLD adn Alzheimer’s
Table of Contents
- 1. Ohio State Researchers Uncover New Pathway in Neurodegeneration Linked to FTLD adn Alzheimer’s
- 2. The Role of GRAMD1B: A New Target for Treatment?
- 3. The Burden of Dementia: FTLD and Alzheimer’s in the U.S.
- 4. Recent Developments and Future Directions
- 5. Practical Applications and Implications for U.S. Readers
- 6. The Future of Dementia Research
- 7. Funding and Support
- 8. What are the potential risks and benefits of modulating GRAMD1B activity for therapeutic purposes?
- 9. Ohio State Researcher dr. Evelyn Reed on Breakthrough in Neurodegeneration Linked to FTLD and Alzheimer’s
- 10. Interview Part 1: The GRAMD1B Revelation
- 11. Interview Part 2: Leveraging “Mini-Brains” and Study Methodology
- 12. Interview Part 3: Therapeutic Avenues and Future Visions
- 13. Interview Part 4: The societal impact and practical steps
- 14. Interview Part 5: Personalized Treatments and Research Landscape
- 15. Interview Part 6: A Call to Action- Reader Discussion
COLUMBUS, ohio – Oct. 26, 2025
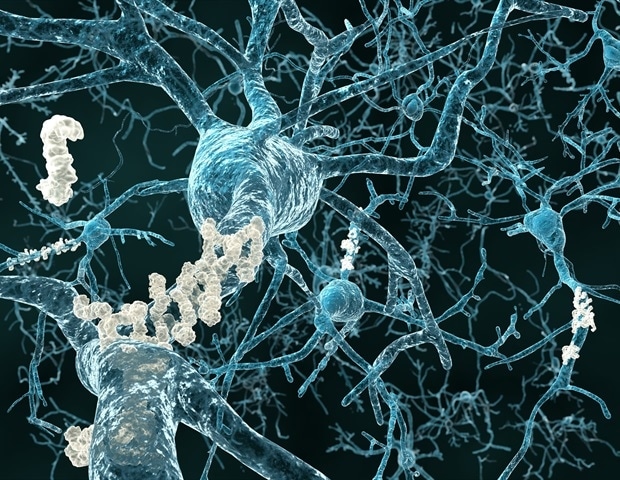
in a notable breakthrough offering new hope in the fight against dementia, researchers at the Ohio State University Wexner Medical Center and College of Medicine have identified a novel mechanism by which neurons behave in neurodegenerative diseases. The study focused on frontotemporal lobar degeneration (FTLD) and Alzheimer’s disease, two of the most prevalent forms of dementia, and utilized human neural organoids – innovative “mini-brain” models derived from FTLD patients – to make their revelation.
This groundbreaking research, published in the journal Nature Communications, sheds light on a previously unknown pathway that could revolutionize the advancement of targeted therapies for these devastating conditions. The findings open a new avenue for understanding the complex molecular processes driving neurodegeneration and offer a potential target for future drug development.
The Role of GRAMD1B: A New Target for Treatment?
The Ohio state team employed cutting-edge techniques to analyze neurons from both human patients and mouse models. A crucial aspect of their methodology was the use of human neural organoids, or “mini-brains,” which replicate the intricate cellular composition of the human brain.This approach allowed the researchers to observe neuronal behavior in a more realistic and relevant context than conventional cell cultures.
Their research pinpointed the protein GRAMD1B as a critical player in regulating cholesterol and lipid storage within neurons.The study revealed that alterations in GRAMD1B levels disrupt the balance of cholesterol, lipid stores, and modified tau protein within these cells. This is particularly significant because imbalances in these elements are strongly associated with the development of both FTLD and Alzheimer’s disease.
Scientists know that GRAMD1B plays a role in other parts of the body like the adrenal gland and intestine but until now the protein has never been studied in the brain. The findings are exciting because by targeting GRAMD1B, we can possibly develop new therapies to help people with FTLD and Alzheimer’s.
Hongjun “Harry” Fu, PhD, study corresponding author, assistant professor of neuroscience at Ohio State
Dr. Fu’s statement underscores the novelty and potential impact of this discovery. While GRAMD1B’s functions in other bodily systems were known, its role in the brain remained a mystery until now. The prospect of targeting GRAMD1B to restore balance in cholesterol and lipid metabolism offers an exciting new therapeutic strategy.
Consider the implications for drug development. if a drug could be designed to modulate GRAMD1B activity, it might be possible to prevent or slow down the progression of these debilitating diseases. This approach aligns with a growing trend in Alzheimer’s research, which seeks to address the underlying biological mechanisms rather than simply treating the symptoms.
The Burden of Dementia: FTLD and Alzheimer’s in the U.S.
The urgency of this research is underscored by the significant impact of FTLD and Alzheimer’s disease on the U.S. population. While FTLD is less common, affecting an estimated 50,000 to 60,000 Americans, Alzheimer’s disease presents a far greater challenge. The Alzheimer’s Association’s 2024 report estimates that approximately 6.9 million Americans aged 65 and older are living with Alzheimer’s dementia.
These numbers are projected to rise dramatically in the coming decades as the U.S. population ages. The financial and emotional toll on families and the healthcare system is immense, highlighting the critical need for effective treatments and preventative strategies.
Recent Developments and Future Directions
The discovery of GRAMD1B’s role in neurodegeneration builds upon a growing body of research exploring the link between lipid metabolism and brain health. Recent studies have also highlighted the importance of inflammation and oxidative stress in the development of Alzheimer’s disease. Understanding how these different factors interact is crucial for developing complete treatment strategies.
the Ohio State team plans to further investigate the specific mechanisms by which GRAMD1B affects cholesterol and tau protein levels. They also aim to explore the potential of targeting GRAMD1B in preclinical studies, using animal models to test the efficacy and safety of potential drugs.
Furthermore, researchers are increasingly focusing on personalized medicine approaches to dementia treatment. This involves tailoring therapies to the individual based on their genetic profile, lifestyle factors, and disease stage. Identifying biomarkers that can predict disease progression is a key aspect of this effort.
Practical Applications and Implications for U.S. Readers
For U.S. readers, this research has several practical implications:
- Increased awareness: Understanding the role of lipid metabolism in brain health can empower individuals to make lifestyle choices that support cognitive function. This includes maintaining a healthy diet, engaging in regular exercise, and managing cholesterol levels.
- Early Detection: Supporting research initiatives that focus on early detection and diagnosis of dementia is crucial. Early intervention can potentially slow down disease progression and improve quality of life.
- Advocacy: Advocating for increased funding for Alzheimer’s and FTLD research can accelerate the development of new treatments and support programs for patients and their families.
- Clinical Trial participation: Consider participating in clinical trials to help advance research and potentially gain access to new therapies.
The Future of Dementia Research
The discovery of GRAMD1B’s role in neurodegeneration represents a significant step forward in the fight against FTLD and Alzheimer’s disease. While much work remains to be done, this research provides a new target for drug development and offers hope for more effective treatments in the future. As the U.S. population continues to age, investing in dementia research and supporting those affected by these devastating diseases is more critical than ever.
Funding and Support
This research was made possible through the support of the BrightFocus foundation’s alzheimer’s disease Research, the National Institute on Aging of the National Institutes of Health, The Ohio State University Chronic Brain Injury Discovery Theme pilot grant, and The Ohio state University Neurological Research Institute seed grant. Continued funding is essential to building on these findings and translating them into tangible benefits for patients and families affected by dementia.
What are the potential risks and benefits of modulating GRAMD1B activity for therapeutic purposes?
Ohio State Researcher dr. Evelyn Reed on Breakthrough in Neurodegeneration Linked to FTLD and Alzheimer’s
Interview Part 1: The GRAMD1B Revelation
Archyde News: Dr. Reed, thank you for joining us.Your team’s recent publication in Nature Communications has made significant waves. Could you briefly explain the core findings regarding GRAMD1B and its role in frontotemporal lobar degeneration (FTLD) and Alzheimer’s disease?
Dr. Evelyn Reed: Thank you for having me. Our research identified GRAMD1B,a protein previously unstudied in the brain,as a key regulator of cholesterol and lipid balance within neurons. We found that disruptions in GRAMD1B levels substantially impact lipid storage and tau protein modification, which are strongly associated wiht both FTLD and Alzheimer’s disease. This opens a novel pathway for therapeutic intervention.
Interview Part 2: Leveraging “Mini-Brains” and Study Methodology
Archyde News: You mentioned the use of human neural organoids,or “mini-brains.” How did this approach contribute to your findings, and what advantages does it offer over customary cell cultures?
Dr. Reed: Human neural organoids were absolutely crucial. Thay allowed us to study neuronal behavior in a more realistic, three-dimensional surroundings, replicating the complex cellular interactions of the human brain.This is far more relevant than studying isolated cells, giving us a more accurate understanding of how GRAMD1B operates within a functioning neural network, especially in patient-derived models.
Interview Part 3: Therapeutic Avenues and Future Visions
archyde News: The prospect of targeting GRAMD1B for therapeutic purposes is exciting. Can you elaborate on how modulating GRAMD1B activity might possibly slow down or prevent the progression of FTLD and Alzheimer’s?
Dr. Reed: If we can develop a drug that effectively modulates GRAMD1B, we could potentially restore balance to cholesterol and lipid metabolism within neurons. this has the potential to mitigate the detrimental effects of tau protein alterations and lipid imbalances, which, in turn, may slow or halt the progression of these diseases by addressing key underlying mechanisms.
Interview Part 4: The societal impact and practical steps
Archyde News: With the rising prevalence of dementia in the U.S.,this research holds immense meaning for the public. How can individuals proactively support the fight against FTLD and Alzheimer’s, and what concrete steps can they take?
Dr. Reed: Awareness is key. Embrace a healthy lifestyle that supports cognitive function, including diet, exercise, and cholesterol management and participate in research trials. Support organizations that fund dementia research and advocate for increased funding. Lastly, prioritize early detection and diagnosis by seeking medical evaluation if you or a loved one experience concerning symptoms.
Interview Part 5: Personalized Treatments and Research Landscape
Archyde News: Looking ahead, what are the next steps for your research team, and what trends are you seeing in the broader field of dementia research, especially regarding personalized medicine?
Dr. Reed: We are currently delving deeper into the specific mechanisms by which GRAMD1B impacts cholesterol and tau protein levels. We also plan to conduct preclinical studies using animal models to test potential drug efficacy and safety. Furthermore, the shift towards personalized medicine is exciting; we are working toward identifying predictive biomarkers to tailor treatments based on individual profiles, which significantly enhance treatment efficacy.
Interview Part 6: A Call to Action- Reader Discussion
Archyde News: Given the potential of these findings, how do you envision the integration of this new treatment pathway with current approaches will shape future Dementia Treatment? Our readers would love to know and we eagerly await their comments
Dr. Reed: That is a great question.I envision an prospect to integrate and enhance present treatments like Lifestyle changes, Early Detection, and personalized medicinal routes. It is a new horizon.