
Men’s Golf: 7th Place Regular Season Finale
FGCU Men’s Golf Finishes Seventh at Lewis Chitengwa Memorial, Eyes ASUN Championship By Archyde News Journalist April 17, 2024 Florida Gulf Coast University’s (FGCU) men’s

FGCU Men’s Golf Finishes Seventh at Lewis Chitengwa Memorial, Eyes ASUN Championship By Archyde News Journalist April 17, 2024 Florida Gulf Coast University’s (FGCU) men’s

Pontevedra’s Saponina store to Close Doors: A reflection on Sustainable Consumption in Spain Saponina, a Pontevedra store specializing in eco-friendly cleaning and hygiene products, is
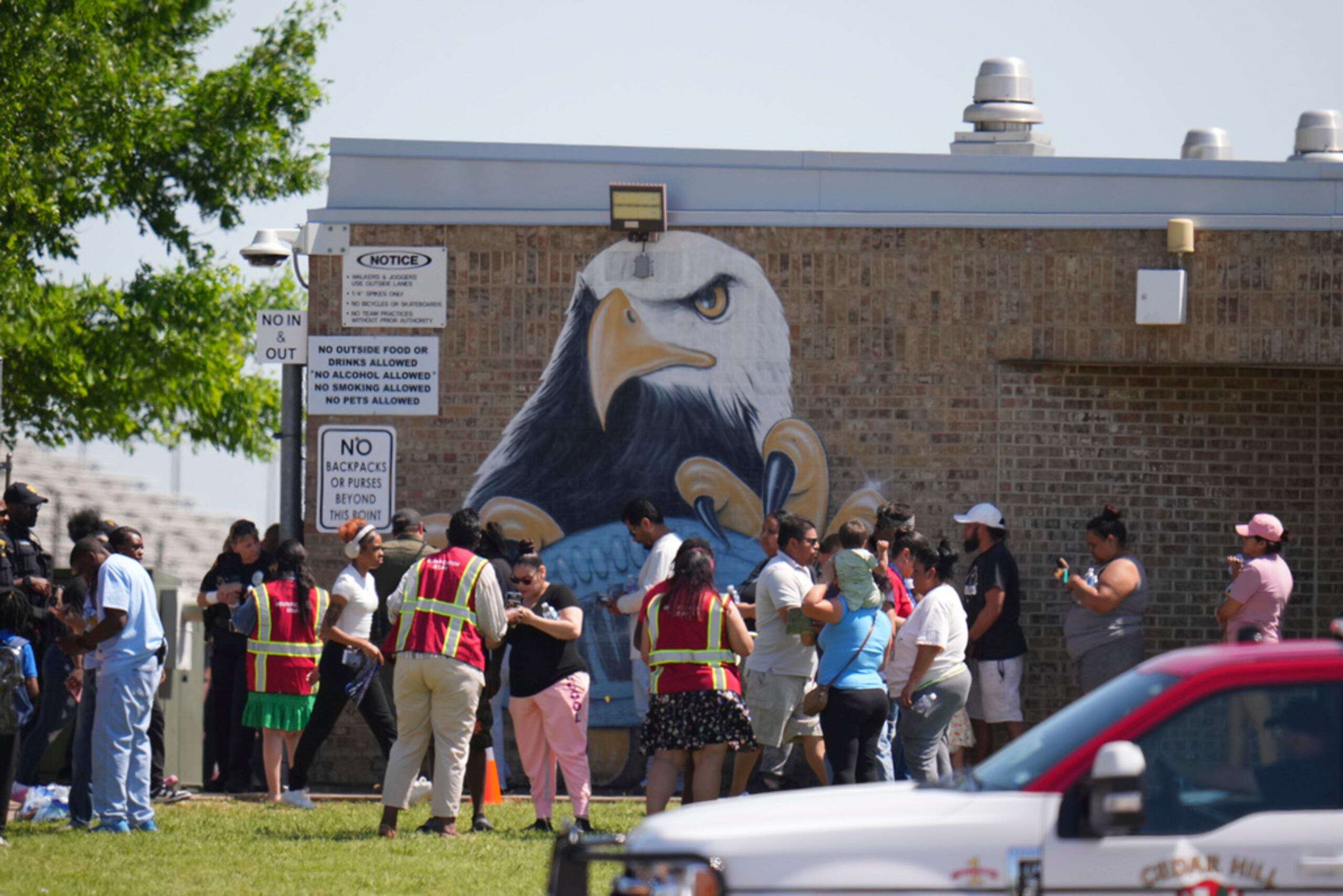
“`html Suspect Arrested After Shooting at Dallas High School Wounds Four Students By Archyde News Published May 14, 2024 DALLAS – A tense afternoon at

U.S. State Department Considers Closing Nearly 30 Embassies and Consulates Amid Cost-Cutting Measures Internal documents reveal potential closures primarily in Europe and Africa, sparking debate

FGCU Men’s Golf Finishes Seventh at Lewis Chitengwa Memorial, Eyes ASUN Championship By Archyde News Journalist April 17, 2024 Florida Gulf Coast University’s (FGCU) men’s

Pontevedra’s Saponina store to Close Doors: A reflection on Sustainable Consumption in Spain Saponina, a Pontevedra store specializing in eco-friendly cleaning and hygiene products, is
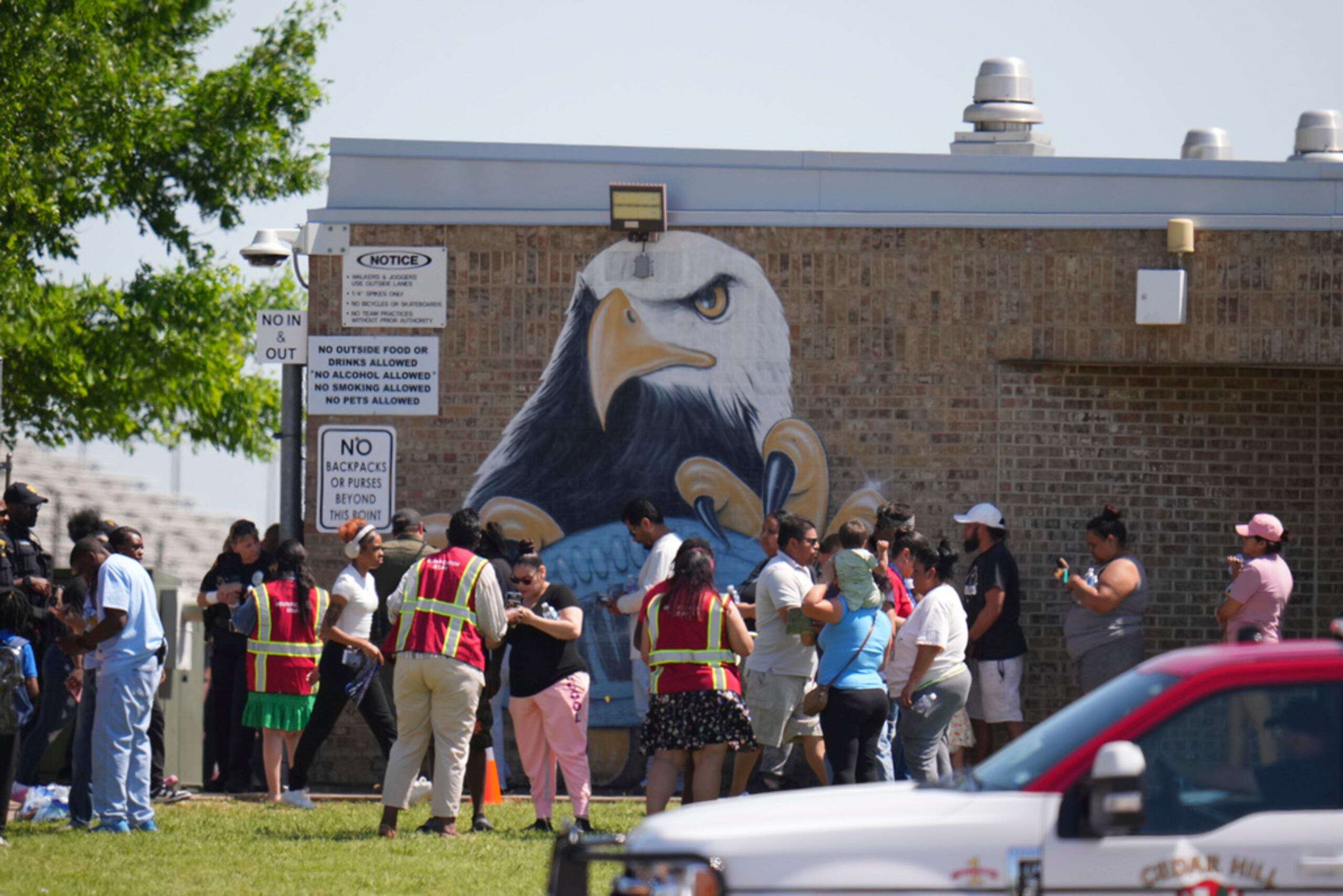
“`html Suspect Arrested After Shooting at Dallas High School Wounds Four Students By Archyde News Published May 14, 2024 DALLAS – A tense afternoon at

U.S. State Department Considers Closing Nearly 30 Embassies and Consulates Amid Cost-Cutting Measures Internal documents reveal potential closures primarily in Europe and Africa, sparking debate

© 2025 All rights reserved