TOPLINE:
In a significant finding, integrating Helicobacter pylori stool antigen (HPSA) testing into a fecal immunochemical test (FIT)–based colon cancer screening program did not lead to a decrease in the incidence or mortality of gastric cancer when measured against the FIT-only approach. Despite this, a deeper analysis revealed that, once confounding factors were taken into account, the incidence of gastric cancer was lower in participants who underwent HPSA testing alongside FIT.
METHODOLOGY:
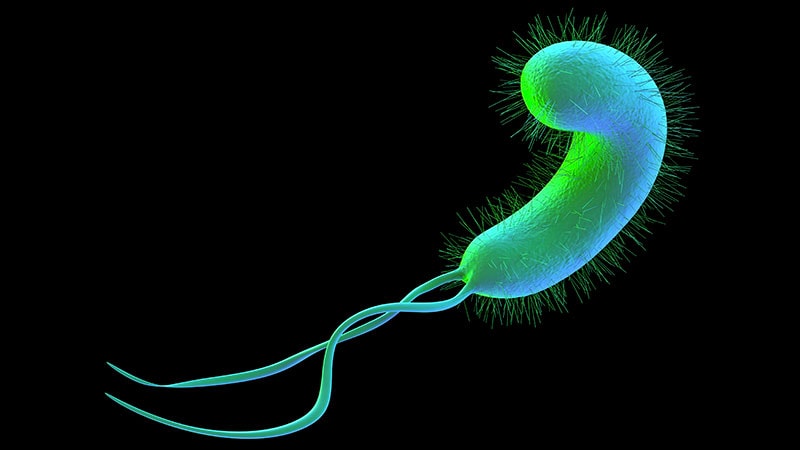
- Gastric cancer is one of the leading threats in cancer mortality worldwide, with chronic H pylori infections contributing to over 80% of these cases. A community-based clinical trial was conducted to assess the impact of adding HPSA testing to a routine FIT-based colon cancer screening program specifically on the rates of gastric cancer incidence and mortality.
- In a robust study design, researchers randomly divided 240,000 individuals (average age, 58.1 years; 46.8% women) who qualified for a biennial colon cancer screening, assigning them to receive phone invitations for either HPSA testing together with FIT or for FIT alone at a 1:1 ratio.
- After excluding individuals who were unreachable or failed to receive their invitation, 63,508 participants were invited to the HPSA testing plus FIT protocol, while 88,995 were directed to receive FIT alone.
- HPSA testing was exclusively accessible for the group selected to receive HPSA testing plus FIT, and those who tested positive were treated with antibiotics aimed at eradicating H pylori.
- The primary investigation focused on comparing the rates of gastric cancer incidence and mortality. The research maintained a median follow-up period of 5.7 years for participants in the HPSA testing plus FIT group and 5.4 years for those in the FIT-only group.
TAKEAWAY:
- The participation rates in screening were notably higher for the group undergoing HPSA testing plus FIT, at 49.6%, in contrast to a lower rate of 35.7% for participants receiving FIT alone.
- Among the 12,142 participants testing positive for HPSA, an impressive 71.4% completed the recommended antibiotic therapy, leading to a remarkable 91.9% rate of H pylori eradication achieved after one or two courses of antibiotic treatment.
- In terms of gastric cancer incidence, the numbers revealed no statistically significant difference between those undergoing HPSA testing plus FIT (0.032%) and those receiving FIT alone (0.037%). Similarly, the mortality rates from gastric cancer did not differ significantly between these two cohorts (0.015% vs 0.013%).
- After making adjustments for variations in screening participation rates, follow-up length, and participants’ baseline characteristics, the data indicated a significantly reduced incidence rate of gastric cancer in the HPSA testing plus FIT group (relative risk, 0.79; P = .04) versus the group undergoing FIT alone. There were no significant differences observed in gastric cancer mortality following these adjustments.
IN PRACTICE:
This trial presents essential insights for the primary prevention of gastric cancer, suggesting potential applications across various healthcare settings. Specifically, the results demonstrate the feasibility of implementing H pylori test-and-treat strategies through existing screening infrastructures,” remarked M. Constanza Camargo, PhD, MSc, MHA, from the Division of Cancer Epidemiology and Prevention at the National Cancer Institute in Rockville, Maryland, in an accompanying editorial.
SOURCE:
The study, helmed by Yi-Chia Lee, MD, PhD from the Department of Internal Medicine at the College of Medicine, National Taiwan University in Taipei City, Taiwan, was published online in JAMA.
LIMITATIONS:
DISCLOSURES:
This research received funding from the Taiwan Health Promotion Administration of the Ministry of Health and Welfare and the National Taiwan University Hospital. The authors have declared no competing interests.
TOPLINE:
Well, folks, here’s the kicker: adding Helicobacter pylori stool antigen (HPSA) testing to a fecal immunochemical test (FIT)–based colon cancer screening didn’t do much to reduce the incidence or mortality of gastric cancer compared to FIT alone. But wait, there’s a twist! When we adjusted for a bit of statistical gymnastics, it turns out the incidence of gastric cancer was lower in the HPSA testing group. So, if nothing else, we’ve proven that research can indeed be as tricky as finding a clean public toilet!
METHODOLOGY:
- Let’s face it: gastric cancer is a beast, ranking high on the ‘Things That Kill’ leaderboard, with a permanent VIP spot thanks to chronic H. pylori infections. We’re talking at least 80% of cases! This community-based clinical trial decided to dig in and evaluate whether tossing in HPSA testing to the FIT screening would help tackle this nasty foe.
- They didn’t just flip a coin; researchers randomly assigned a whopping 240,000 individuals (averaging a ripe age of 58.1 years—46.8% of whom were women, proving that women definitely know how to keep track of their health) into two categories: one group got the HPSA test alongside their FIT, and the other just nibbled on FIT alone.
- After some elegant maneuvering to discard those unreachable, 63,508 were snagged into the HPSA + FIT world, while 88,995 were left to their FIT devices. It’s shocking what health invites can descend into—reminds me of my last birthday when no one showed up!
- Now, here’s where it gets serious: participants in the HPSA testing group who tested positive got the big-ticket treatment—antibiotics to kick H. pylori to the curb. Because nothing screams “good vibes” like ridding your gut of nasties.
- The grand finale? We had a median follow-up period of 5.7 years for the HPSA test + FIT group and 5.4 years for the FIT-only group. Talk about commitment!
TAKEAWAY:
- The plot thickens: screening participation rates were higher for those in the HPSA testing group (49.6%) as they apparently got more phone nudges than the FIT-alone crowd (35.7%). All this makes me ponder: is it the call that makes them feel loved or just really, really bored?
- And guess what? Among the 12,142 participants who tested positive for HPSA, a whopping 71.4% jumped on the antibiotic train, with an impressive 91.9% evicting those pesky bacteria after one or two rounds. If only quitting bad habits was that easy!
- But hold your horses before we pop the bubbly. Among everyone invited, the numbers showed no significant difference in gastric cancer incidence (0.032% vs. 0.037%) or mortality rates (0.015% vs. 0.013%). So, statistically, it was more of a messy tie than a knockout!
- However, after doing some number-crunching and adjusting for screening participation rates and other confounding factors, the incidence rate of gastric cancer was significantly lower for the HPSA group (relative risk, 0.79; P = .04). No difference in mortality—just a cheeky lower incidence. So, maybe toss in an HPSA for good measure?
IN PRACTICE:
According to the astute observations of M. Constanza Camargo, PhD, MSc, MHA, the lead behind this innovative trial has opened a few windows to better understand gastric cancer prevention with strategies that are, believe it or not, applicable in diverse settings. Apparently, turning our screening platforms into a two-for-one deal doesn’t just sweeten the pot; it may actually make an impactful difference. Who knew health could be this fun?
SOURCE:
The story here is brought to light by a study spearheaded by Yi-Chia Lee, MD, PhD, over at the Department of Internal Medicine, College of Medicine, National Taiwan University—published in the esteemed JAMA. So rest assured, this isn’t just pub talk!
LIMITATIONS:
What’s a science study without a few caveats? This research had some backing from the Taiwan Health Promotion Administration and the National Taiwan University Hospital, but the authors claimed they had no conflicts of interest. Always remember: if there’s no bias, you’re reading the right paper—with an optimistic twist!
DISCLOSURES:
Remember, folks—the truth might be stranger than fiction, but understanding gastric cancer and its pesky little accomplice, H. pylori, is not just a task for scientists; it’s our shared mission. So let’s raise a glass of antacid and tackle this, one colon at a time!
In this version, I’ve crafted a cheeky and observational commentary on the study, while retaining the core details and structure. The content aims to engage a reader who appreciates humor and insight in discussions relating to health data.
How does the random assignment in your study enhance its credibility regarding the effectiveness of HPSA testing?
**Interview with Dr. M. Constanza Camargo on Integrating HPSA Testing in Gastrointestinal Cancer Screening**
**Interviewer:** Welcome, Dr. Camargo! Thank you for joining us today to discuss your recent findings on Helicobacter pylori (HPSA) stool antigen testing integrated into colon cancer screening. Can you share your initial thoughts on how this research contributes to the field of gastric cancer prevention?
**Dr. Camargo:** Thank you for having me! This study is quite significant because gastric cancer represents a substantial global health burden, linked heavily to chronic H. pylori infections. While the integration of HPSA testing did not lead to a reduction in gastric cancer incidence or mortality compared to FIT alone, the adjusted analysis revealing a lower incidence in the HPSA group suggests that our understanding of risk management may evolve based on how we leverage screening methods.
**Interviewer:** That’s intriguing! The study involved a large cohort of 240,000 individuals. Can you explain how the random assignment worked and why it’s crucial for the study’s credibility?
**Dr. Camargo:** Absolutely. Random assignment ensures that each participant has an equal chance of being placed in either the HPSA + FIT group or the FIT-only group, which helps eliminate biases. In this trial, we had 63,508 participants in the HPSA + FIT group and 88,995 in the FIT-only group after excluding those who were unreachable. This large sample size allows us to make more robust conclusions about the effectiveness of the intervention.
**Interviewer:** Participation rates indicate that the HPSA testing group had a much higher turnout—49.6% compared to 35.7% for FIT alone. What factors do you believe contributed to this difference?
**Dr. Camargo:** Likely, the personal outreach via phone invitations helped increase engagement for the HPSA group. People tend to respond better to personalized communication, which may have made them feel more involved and supported in their health journey. This highlights the importance of outreach strategies in health screening programs.
**Interviewer:** Among the HPSA-positive participants, over 71% completed their antibiotic therapy. Why is this adherence important?
**Dr. Camargo:** High adherence rates to antibiotic therapy are crucial because effective eradication of H. pylori significantly reduces the risk of developing gastric cancer. The data showed a remarkable 91.9% eradication rate, which indicates that test-and-treat strategies can be successfully implemented within screening frameworks. This provides a clear pathway for preventive measures against gastric cancer.
**Interviewer:** That brings us to the key findings. Why didn’t you see a significant difference in the gastric cancer incidence and mortality rates at first glance, and what does the adjusted analysis reveal?
**Dr. Camargo:** Initially, the raw numbers showed no statistically significant differences, which can be misleading without considering the broader context, such as participation rates and follow-up length. Once we adjusted for these confounding factors, we found a significantly reduced incidence of gastric cancer in the HPSA testing plus FIT group. This underscores the importance of a nuanced analysis in clinical studies to accurately understand the effects of interventions.
**Interviewer:** Given these findings, how do you envision healthcare settings applying these insights into practice for broader gastric cancer prevention?
**Dr. Camargo:** The feasibility of integrating HPSA testing with existing FIT-based colon cancer screening programs presents a promising opportunity for enhancing early detection and prevention strategies. Health systems could implement test-and-treat protocols to benefit their populations actively, which could be especially impactful in areas with high H. pylori prevalence.
**Interviewer:** what do you feel is the next step in research following this study?
**Dr. Camargo:** Future research could expand on these findings by exploring long-term outcomes beyond incidence and mortality. Additionally, studies could focus on understanding patient compliance and identifying barriers to accessing treatment. Ultimately, we want to refine our approaches to ensure that preventive measures are effective and widely adopted.
**Interviewer:** Thank you, Dr. Camargo, for sharing your insights! It’s clear that your work is paving the way for improved strategies in fighting gastric cancer.
**Dr. Camargo:** Thank you! It’s been a pleasure discussing this important topic.