A Rare Phenomenon: Mistaking Immune Response for Treatment Failure in Invasive Fungal Infection
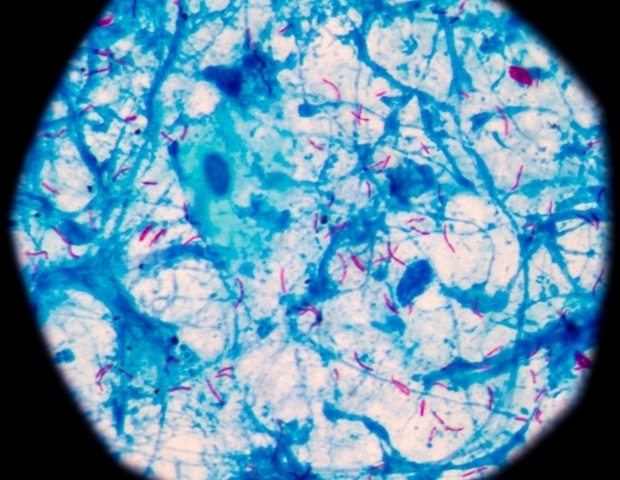
Invasive pulmonary Aspergillus infection, a serious complication following influenza, can pose significant challenges in diagnosis and treatment. A recent case highlights the importance of recognizing a rare but critical phenomenon known as immune reconstitution inflammatory syndrome (IRIS) which can mimic treatment failure.
The patient in this case presented with invasive pulmonary Aspergillus infection after being infected with Influenza A Virus (IAV). Despite receiving active antifungal therapy, the patient’s clinical symptoms surprisingly worsened, and lung imaging showed progressive lesions. However, laboratory indicators showed improvement, which suggested the possibility of IRIS.
IRIS is a paradoxical inflammatory response that occurs after the initiation of effective treatment for underlying infections like tuberculosis or, in this case, invasive fungal infections. This inflammatory response can be severe, resembling a worsening of the original infection, and can lead to confusion and misdiagnosis.
“Increased clinical manifestations combined with increased lung imaging findings during antifungal therapy are often misjudged as failure of antifungal therapy, and should be vigilant against immune reconstitution inflammatory syndrome,” says Dr. [Insert Author Name Here].
In this particular case, the patient’s clinical presentation pointed towards IRIS. While symptoms worsened and imaging suggested disease progression, the improvement in laboratory indicators acted as a crucial piece of the puzzle, hinting at an immune system actively battling the infection.
The recognition of IRIS is crucial for several reasons. Firstly, it can prevent unnecessary changes in antifungal therapy due to the perceived lack of response. Such changes can lead to the development of drug resistance, making future treatments more challenging. Secondly, understanding IRIS allows for appropriate management strategies to be implemented, mitigating the potentially serious inflammatory complications.
The case emphasizes the need for a thorough and nuanced understanding of the various mechanisms at play in infectious diseases. Recognizing IRIS as a potential differential diagnosis, particularly in patients with immunocompromised systems, could significantly improve treatment outcomes and ultimately save lives.
The present case highlights the importance of a multidisciplinary approach to managing complex fungal infections. The need for close collaboration between clinicians, microbiologists, and radiologists is critical to ensure timely and accurate diagnosis and treatment.
Further research is needed to better understand the pathogenesis of IRIS and to develop specific diagnostic and treatment modalities. This will help clinicians to recognize and manage this complex immune phenomenon effectively.
For patients with suspected invasive fungal infections, it’s essential to communicate openly with your healthcare providers about your symptoms and any concerns you may have. By working together, we can strive for the best possible outcome.
Keywords:
Aspergillus infection, Influenza A Virus, Immune Reconstitution Inflammatory Syndrome, IRIS, Antifungal therapy,
What are the key clinical signs that might differentiate IRIS from actual treatment failure in invasive fungal infections?
## A Rare Phenomenon: Mistaking Immune Response for Treatment Failure in Invasive Fungal Infection
**Interviewer:** Welcome, Dr. [Insert Alex Reed Name Here]. Today we’re discussing a fascinating and potentially dangerous phenomenon known as Immune Reconstitution Inflammatory Syndrome, or IRIS, in the context of invasive fungal infections.
**Dr. Alex Reed:** Thank you for having me. IRIS is indeed a fascinating and sometimes tricky phenomenon to recognize.
**Interviewer:** Can you explain what IRIS is in layman’s terms and how it can complicate the treatment of invasive fungal infections?
**Dr. Alex Reed:** Imagine your immune system as an army fighting off infection. When someone has a weakened immune system, like after battling influenza, they become more vulnerable to infections like Aspergillus. Now, when we start treating these infections with antifungal medication, it’s like sending reinforcements to the army.
IRIS occurs when this ”reinforcement” – the effective treatment – triggers a potent inflammatory response. The body, essentially, overreacts to the dying infection. This can lead to worsening symptoms and even changes in imaging, making it look like the treatment isn’t working, when in fact, the body is just enthusiastically clearing the infection. [[1](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7651489/)]
**Interviewer:** That sounds counterintuitive – wouldn’t a worsening condition indicate treatment failure?
**Dr. Alex Reed:** That’s the tricky part. IRIS can definitely mimic treatment failure. However, there are often clues that point towards IRIS instead. We see a disconnect between clinical symptoms and lab results. For example, a patient might feel worse, their lung images might show more lesions, but their inflammatory markers in the blood improve. This discrepancy can be a red flag for IRIS.
**Interviewer:** So, what should clinicians be looking out for to avoid misdiagnosing IRIS as treatment failure?
**Dr. Alex Reed:** Awareness is key! Clinicians need to be aware of IRIS as a possibility, especially in patients with a history of weakened immune systems who are showing improvement in laboratory markers despite worsening clinical symptoms and imaging.
It’s important to carefully evaluate the overall clinical picture, considering all the available data before assuming treatment failure. Early recognition of IRIS allows for appropriate management and prevents unnecessary changes in therapy. [[1](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7651489/)]
**Interviewer:** Thank you, Dr. Alex Reed for shedding light on this complex issue.
I’m sure this information will be invaluable to both healthcare professionals and the public.