Balancing Act: Scientists Discover How to Fine-Tune T-Cells for Targeted Cancer Immunotherapy
By a Senior Staff Writer
For nearly two decades, researchers have been striving to refine cancer immunotherapy, seeking ways to make it more effective while minimizing harm to healthy tissues. Now, a collaborative team led by researchers at the U.S. National Cancer Institute (NCI) and the University of Montreal (UdeM) has achieved a significant breakthrough. their findings, published in the prestigious journal Cell, reveal a novel approach to modulating the immune system’s response, potentially paving the way for more targeted and safer cancer treatments.
A 20-Year Journey into Immune Cell Dynamics
“This story goes back nearly 20 years,” explains Prof. Paul François, a biophysicist and bio-informaticist at UdeM. His work focuses on applying mathematical models to understand complex biological processes. His journey into immunology began with a pivotal seminar led by Franco-American immunologist grégoire Altan-Bonnet from the National Cancer Institute (NCI) in the U.S.. Prof. François recalls, “From a mathematical viewpoint, I didn’t understand what was going on.So I developed an interest in the immune system.” This initial curiosity sparked a long and fruitful collaboration.
Working with Dr. Altan-Bonnet, immunologist Naomi Taylor (also of the U.S. NCI), and their respective teams, Prof. François contributed to a project that culminated in a groundbreaking finding. Key contributors to this research included François Bourassa, Sooraj Achar, and Taisuke Kondo.
prof. François emphasizes the collaborative nature of the project: “It’s really a team effort.” The team utilized a cutting-edge robotics platform – “akin to an immune system microscope” – developed in Dr. Altan-Bonnet’s lab in collaboration with Prof.François, allowing them to meticulously study the interactions between immune cells and cancer cells. this detailed analysis enabled the creation of a mathematical model that accurately predicted immune responses observed in the lab.
The Promise and Peril of CAR-T Cell Therapy
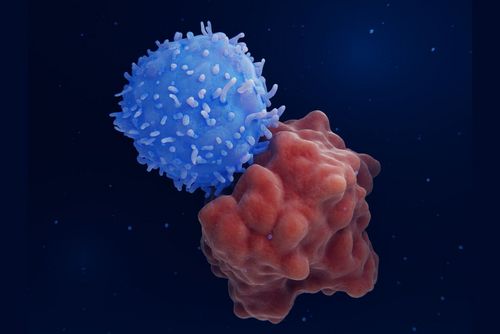
CAR-T cell immunotherapy has emerged as a game-changer in cancer treatment. This approach,often used in conjunction with traditional therapies like chemotherapy and radiotherapy,involves reprogramming a patient’s T-cells – the immune system’s “warriors” – to specifically target and destroy cancer cells. Prof. François likens it to “immune system judo.”
The process involves modifying T-cells in the lab by adding a synthetic chimeric antigen receptor (CAR). this receptor directs the T-cells to attack cancer cells,but the mechanism isn’t always precise. This lack of specificity can lead to T-cells attacking healthy tissue, causing severe side effects. While CAR-T cell therapy has proven highly effective against leukemia, where the consequences of off-target effects are manageable, it faces challenges in treating solid tumors, such as ovarian cancer.
“CAR-T cells attack tumors in the ovaries, but they also destroy the patient’s healthy tissues, particularly the lungs. You attack the cancer, but you kill the patient,” Prof.François explains, highlighting the critical need for a more refined approach.
TCRs as Brakes: A Novel Approach to Fine-Tuning Immune Response
The research team focused on leveraging the natural receptors present in T-cells, known as T-cell receptors (TCRs). Unlike CARs, TCRs can distinguish between healthy and cancerous cells by recognizing subtle differences in the proteins displayed on their surfaces. The challenge, however, is that TCRs are often not potent enough to effectively combat tumors on their own.
the researchers ingeniously combined the benefits of both CARs and TCRs by engineering CAR-T cells that also incorporate TCRs. Their breakthrough lies in discovering that TCRs can act as a “brake,” moderating the CAR cells’ aggressive response and preventing them from attacking healthy tissues. As Prof. François notes, “It was long thought that the TCRs were exclusively ‘accelerators,’ but we showed they could be modulated to suppress the immune response rather of activating it.”
Prof.François and his student François bourassa developed a theoretical mathematical model to guide their efforts,determining how to best modulate the immune response using these naturally occurring receptors. Their model revealed a crucial insight: “To obtain a better immune response, you have to balance out the T-cell’s brake and gas pedals.”
This concept led to the development of an immunotherapy strategy called AEBS (Antagonism-Enforced Braking System). According to Prof. François, “We’re not the only ones who have tried to reprogram CAR cells to make them more effective on tumors, but we’re the first ones to use natural receptors as the brake.” This novel approach allows the engineered T-cells to ease off when encountering healthy tissue while simultaneously intensifying their attack on tumors.
Real-World Applications and Future Directions
The implications of this research are significant. By incorporating naturally occurring receptors as a “brake” on CAR-T cells,scientists can potentially develop more targeted and safer immunotherapies for a wider range of cancers,including solid tumors that have been challenging to treat with existing CAR-T cell therapies. This could lead to treatments with fewer side effects and improved outcomes for patients.
Consider the case of ovarian cancer, which affects over 19,000 women in the U.S. each year. Current treatment options, including surgery and chemotherapy, can be effective, but recurrence is common. CAR-T cell therapy holds promise for treating ovarian cancer, but its submission has been limited by toxicity to healthy tissues. The AEBS system could potentially overcome this limitation, allowing for more effective and targeted treatment of ovarian cancer with fewer side effects.
Moreover, this research opens new avenues for understanding and manipulating the immune system. The mathematical model developed by Prof. François and his team provides a framework for designing and optimizing immunotherapies for a variety of diseases, not just cancer. This could lead to new treatments for autoimmune disorders, infectious diseases, and other conditions where the immune system plays a central role.
Currently, a patent application is in process, and preparations are underway for potential clinical trials. “We started off with a fairly theoretical problem and ended up using the idea to develop a treatment,” Prof. François concludes, emphasizing the tangible impact of this long-term research effort.
Potential Benefits of AEBS Immunotherapy
| Benefit | Description | potential Impact |
|---|---|---|
| Reduced Toxicity | TCRs act as a “brake,” preventing CAR-T cells from attacking healthy tissue. | Fewer side effects for patients,improved quality of life. |
| Increased Specificity | TCRs can distinguish between healthy and cancerous cells, leading to more targeted therapy. | More effective tumor destruction, reduced risk of recurrence. |
| Wider Applicability | AEBS can be applied to solid tumors, which have been difficult to treat with existing CAR-T cell therapies. | Expanded treatment options for patients with various types of cancer. |
| Optimized Immune Response | The mathematical model provides a framework for fine-tuning the immune response. | More effective and durable immune control of cancer. |
Considering the progress in this field, what do you think will be the biggest challenge facing cancer immunotherapy in the next five years, and how can researchers overcome this issue?
balancing Act: An Interview with Professor Paul François on Revolutionizing Cancer Immunotherapy
Archyde News Editor: Welcome, Professor François. It’s a pleasure to have you here today to discuss this groundbreaking research published in Cell. For our readers, could you briefly explain the core concept behind your team’s work on fine-tuning T-cells for cancer immunotherapy?
Prof. Paul François: Thank you for having me.Our research focuses on making CAR-T cell therapy, a type of immunotherapy, more precise. We’re using naturally occurring T-cell receptors, or TCRs, as a “brake” to prevent the CAR-T cells from attacking healthy tissues while enhancing their ability to target and destroy cancer cells.It’s like adding a safety mechanism to target the tumors.
Archyde News Editor: This sounds incredibly complex. Could you elaborate on the challenges of existing CAR-T cell therapy,especially concerning the side effects in solid tumors like ovarian cancer?
Prof. Paul François: Certainly.CAR-T cell therapy has shown remarkable success, especially in treating leukemia. However, it’s less effective and more problematic with solid tumors. The CAR-T cells,engineered to target cancer cells,sometiems also attack healthy tissues,causing severe side effects. For example,in ovarian cancer,they might affect the lungs. This is what we aimed to improve upon using our AEBS (Antagonism-Enforced Braking System) approach.
Archyde News Editor: The growth of the AEBS system is captivating. Could you break down how TCRs function as a “brake” and how this enhances the therapy’s specificity?
Prof. Paul François: We discovered that TCRs, wich naturally recognize proteins on both healthy and cancerous cells, can be modulated. By incorporating TCRs into the CAR-T cells, we could essentially tell the cells, “ease off when you encounter healthy tissue.” Meanwhile, the CAR component still ensures that they stay focused on the cancer cells. This dual action considerably increases the specificity.
Archyde News Editor: Your team utilized a mathematical model to guide this process. Could you shed some light on how this model was created and its role in achieving such a breakthrough?
Prof. Paul François: Absolutely. We developed a mathematical model leveraging data generated through cutting-edge robotics research to understand the interaction between immune cells and tumors. The model enabled us to predict and optimize the immune response by effectively balancing the “accelerator” and “brake” functions of the T-cells. This was essential in understanding and fine-tuning the immune response.
Archyde News Editor: The implications seem substantial, especially for solid tumors like ovarian cancer. What impact do you foresee the research having on cancer treatment in the future?
prof. Paul François: We are optimistic that our AEBS system will lead to more targeted and safer immunotherapies. This could pave the way for using CAR-T cell therapy in a broader range of cancers,especially solid tumors,while reducing side effects. We hope it will eventually lead to better treatment outcomes for patients.
Archyde News Editor: What’s next for this research? Are clinical trials on the horizon?
Prof. Paul François: Yes, we have a patent submission in progress, and we are preparing for future clinical trials. We’re excited about the potential real-world impact, taking this from being a theoretical problem to actually developing a treatment for cancer patients.
Archyde News Editor: This is truly exciting work, Professor. Considering the progress in this field, what do you think will be the biggest challenge facing cancer immunotherapy in the next five years, and how can researchers overcome this issue?
Prof.Paul François: One notable challenge will be translating these lab successes into reliable and widely available therapies.Developing more elegant clinical trial design and the ability to scale up production while maintaining effectiveness and safety are all key. Collaboration, knowledge sharing, and technological advancements are crucial to overcoming these hurdles.
Archyde News Editor: Thank you, Professor François, for sharing your insights. This is clearly a significant advancement in the quest to make cancer immunotherapy more effective and less harmful. Our readers at Archyde will surely be interested in the continued evolution of this critically importent research.
Prof. Paul François: Thank you for having me. it’s been a pleasure discussing this work.