Early Ambulation After Hip Fracture Surgery linked to Improved Walking recovery: Insights from a Japanese Study
Table of Contents
- 1. Early Ambulation After Hip Fracture Surgery linked to Improved Walking recovery: Insights from a Japanese Study
- 2. The Impact of Early Ambulation on Recovery
- 3. Study Design and Methodology
- 4. Ethical Considerations
- 5. Key Measurements and Variables
- 6. Key Findings: Early Ambulation Leads to Better Outcomes
- 7. Implications for U.S. Rehabilitation Practices
- 8. Addressing Potential Counterarguments
- 9. Conclusion: A Promising Path to Improved Hip Fracture Recovery
- 10. Early Ambulation After Hip Fracture Surgery Significantly Improves Walking Ability: New Insights
- 11. The Link Between early Ambulation and Walking Independence
- 12. Beyond Early Ambulation: Key Factors Affecting Recovery
- 13. Statistical Analysis and Methodology
- 14. Practical Implications for U.S. Healthcare
- 15. Recent Advances in Hip Fracture Care
- 16. Addressing Potential Concerns
- 17. Conclusion: A Path to Improved Recovery
- 18. Early Ambulation After Hip Fracture Surgery Linked to Improved Walking Independence
- 19. The Importance of Early Mobility
- 20. Study Design and Methodology
- 21. Subgroup Analyses: Understanding Specific Patient Groups
- 22. Statistical software
- 23. Practical Applications and Implications for U.S. Healthcare
- 24. Potential Counterarguments and Considerations
- 25. Recent Developments and Future Research
- 26. ]
- 27. Interview: Dr. Evelyn reed on Early Ambulation After Hip Fracture Surgery
- 28. Introduction
- 29. The Meaning of Early Ambulation
- 30. Key Findings from the Japanese Study
- 31. Implications for U.S. Healthcare
- 32. Addressing Potential Concerns
- 33. Future Research and Developments
- 34. Call To Action
- 35. Reader Engagement
- 36. Conclusion
A recent study in Japan sheds light on the benefits of early ambulation following hip fracture surgery, offering valuable insights for rehabilitation practices in the U.S.
The Impact of Early Ambulation on Recovery
Hip fractures are a significant health concern, especially among older adults. In the United States, the Centers for Disease Control adn Prevention (CDC) estimates that approximately 300,000 people are hospitalized each year due to hip fractures, with a significant portion of thes cases occurring in individuals aged 65 and older. These fractures can lead to decreased mobility, reduced independence, and a higher risk of complications.
A new study published recently investigated the impact of early ambulation – that is, starting to walk soon after surgery – on the recovery of walking ability in elderly patients who have undergone hip fracture repair. The study, conducted in Japan, offers compelling evidence that early ambulation can lead to better outcomes.
“This study highlights the importance of timely rehabilitation interventions in optimizing functional recovery after hip fracture surgery.”
The findings of this study have implications for rehabilitation protocols in the U.S., where healthcare providers are continuously seeking ways to improve patient outcomes and reduce healthcare costs associated with hip fracture recovery.
Study Design and Methodology
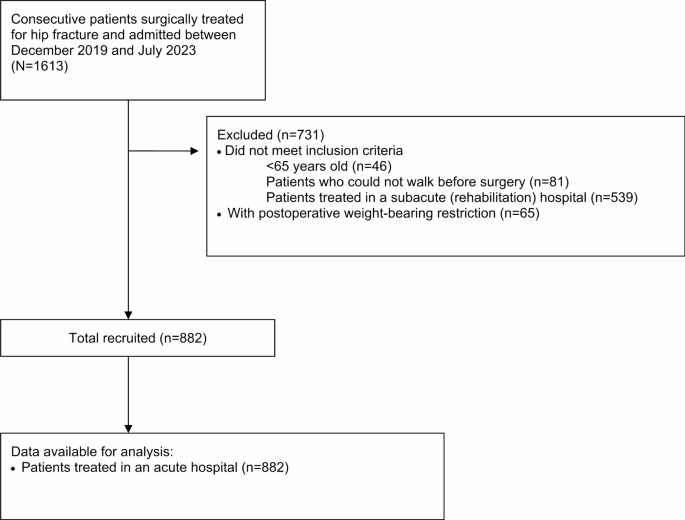
The multicenter cohort study, utilizing the Nagano hip fracture database in Japan, examined data from 1613 surgically treated patients across 17 hospitals between December 1, 2019, and July 31, 2023. The inclusion criteria focused on ambulatory patients aged 65 or older with femoral neck or trochanteric fractures who were admitted to acute care hospitals.patients with postoperative weight-bearing restrictions were excluded.
This rigorous approach ensured a focused analysis of the impact of early ambulation in a relevant patient population. The data, collected via a cloud-based electronic system, encompassed a wide range of patient characteristics and medical factors, offering a comprehensive view of the recovery process.
Patients’ recruitment and flow diagram.
Ethical Considerations
The study was conducted in accordance with the Declaration of Helsinki, ensuring the protection of patient rights and welfare.The Ethics Committee of the School of Medicine, Shinshu University, approved the study on November 12, 2019 (protocol number: 4541). Informed consent was waived due to the observational nature of the study, but an opt-out approach was implemented, allowing patients to decline participation. Detailed study information was publicly available through the University Hospital Information Network (UMIN-CTR,unique identifier: UMIN000054114).
Key Measurements and Variables
The database included extensive patient information, such as age, sex, BMI, medical history (respiratory, cardiovascular, neurological diseases), cognitive function, pre-injury mobility, living situation, fracture type, surgical procedure, complications, waiting times for surgery and rehabilitation, and rehabilitation details (time to first ambulation and intervention time).
Cognitive function was assessed using the Degree of Daily Life Independence Score for People with Dementia (DDLIS-PD), a widely used tool in Japan. Cognitive impairment was defined as a DDLIS-PD grade II or higher. Functional Independence Measure (FIM) scores were assessed at multiple points post-surgery to track patient progress.
Dependent Variables:
- Independent walking (FIM grade ≥ 5)
- Walking recovery (restoration of pre-fracture walking status)
- FIM score at discharge
- Walking status at discharge
- Days from operation to discharge
Independent Variable:
- Timing of postoperative ambulation: Early Ambulation (EA) group (postoperative day 1 or 2) vs. Late ambulation (LA) group (postoperative day 3 or later).
The cut-off point for early vs.late ambulation was determined through Receiver Operating Characteristic (ROC) analysis.
Key Findings: Early Ambulation Leads to Better Outcomes
The study’s primary finding was that early ambulation is associated with a substantially higher likelihood of independent walking at discharge. Patients in the EA group demonstrated better functional outcomes compared to those in the LA group.
Specifically, the researchers found that initiating ambulation on postoperative day 1 or 2 was linked to:
- Increased likelihood of achieving independent walking (FIM grade ≥ 5) at discharge.
- Improved overall walking status at discharge (e.g., walking without aids or with a cane).
- Potentially shorter hospital stays, although this outcome requires further investigation.
These findings align with previous research highlighting the benefits of early mobilization in promoting faster recovery and reducing the risk of complications after surgery.
Implications for U.S. Rehabilitation Practices
The results of this study have vital implications for rehabilitation practices in the United States. Given the large number of hip fractures occurring annually in the U.S.,implementing strategies to improve recovery outcomes is crucial.
Here are some potential applications of the study’s findings in the U.S. healthcare system:
- Re-evaluating Post-operative Protocols: Hospitals and rehabilitation centers should consider re-evaluating their post-operative ambulation protocols to encourage earlier mobilization, when medically appropriate.
- Patient Education: Educating patients and their families about the benefits of early ambulation can help promote adherence to rehabilitation plans.
- Resource Allocation: Healthcare facilities may need to allocate additional resources,such as physical therapists and nursing staff,to support early ambulation programs.
- Further Research: Additional research is needed to confirm these findings in diverse U.S. populations and to identify specific interventions that can optimize the benefits of early ambulation.
For example,the Veteran’s Health Administration (VHA),the largest integrated health care system in the United States,could implement system-wide changes based on these findings. The VHA treats a significant number of elderly patients, and improving hip fracture recovery rates could lead to substantial cost savings and improved quality of life for veterans.
Addressing Potential Counterarguments
While the study provides compelling evidence for the benefits of early ambulation, it’s important to address potential counterarguments. Some healthcare providers may be hesitant to implement early ambulation protocols due to concerns about patient safety, pain management, or the availability of resources.
It’s crucial to emphasize that early ambulation should always be implemented under the guidance of qualified healthcare professionals and tailored to the individual needs of each patient.Pain management strategies and appropriate assistive devices should be used to ensure patient comfort and safety. Moreover, healthcare facilities may need to invest in training and resources to support early ambulation programs effectively.
Conclusion: A Promising Path to Improved Hip Fracture Recovery
This study from japan provides valuable evidence supporting the benefits of early ambulation following hip fracture surgery. By implementing evidence-based practices, such as early ambulation protocols, the U.S. healthcare system can strive to improve patient outcomes, reduce healthcare costs, and enhance the quality of life for older adults recovering from hip fractures.
Early Ambulation After Hip Fracture Surgery Significantly Improves Walking Ability: New Insights
Hip fractures are a major health concern, particularly among older adults in the United States. According to the Centers for Disease Control and Prevention (CDC), approximately 300,000 older adults are hospitalized each year for hip fractures. The consequences can be devastating, leading to decreased mobility, loss of independence, and even increased mortality.A crucial goal after hip fracture surgery is regaining the ability to walk independently. Now, a new study sheds light on the importance of early ambulation – starting to walk soon after surgery – in achieving this goal.
The Link Between early Ambulation and Walking Independence
The study underscores the importance of early ambulation in a patient’s recovery journey.Initiating ambulation, defined as walking, on postoperative day 1 or 2, has been shown to significantly improve the likelihood of regaining walking independence.
This finding is particularly relevant in the U.S.,where healthcare systems are increasingly focused on optimizing patient outcomes and reducing hospital stays. Early ambulation aligns with these goals by promoting faster recovery and potentially decreasing the need for long-term care.
Beyond Early Ambulation: Key Factors Affecting Recovery
While early ambulation is crucial, it’s not the only factor determining a patient’s recovery. Several pre-existing conditions and circumstances can significantly impact the ability to walk independently after hip fracture surgery. These include:
- Pre-fracture walking ability: A patient’s mobility before the fracture is a strong indicator of their potential for recovery. Those who were more active before the fracture are more likely to regain their walking ability.
-
Cognitive impairment: Cognitive issues can hinder a patient’s ability to follow instructions and participate in rehabilitation, impacting their recovery.
Impact of prefracture cognitive impairment and postoperative delirium on recovery after hip fracture surgery.
- Preoperative medical history: Existing conditions, such as respiratory, circulatory, and neurological diseases, can complicate recovery.
- Fracture type: The type and severity of the hip fracture can influence the surgical approach and subsequent recovery.
- Days from admission to surgery: Delays in surgery can negatively impact outcomes.
Statistical Analysis and Methodology
The study employed rigorous statistical methods to analyze the data and draw conclusions. Continuous variables, such as age and length of hospital stay, were analyzed using non-parametric methods like the Mann-Whitney U test due to deviations from normality. categorical variables, such as gender and fracture type, were compared using Pearson’s chi-squared test and Fisher’s exact test when expected frequencies were low.
To pinpoint the optimal cutoff for early ambulation, a Receiver Operating Characteristic (ROC) analysis was conducted. The Youden index was utilized to determine the threshold that best distinguished between patients who achieved walking independence and those who did not. The robustness of this cutoff was then assessed through stratified analysis across different patient subgroups.
Practical Implications for U.S. Healthcare
The findings of this study have several practical applications for healthcare professionals in the U.S.:
- Early mobilization protocols: Hospitals and rehabilitation centers should implement protocols that prioritize early ambulation for hip fracture patients, when medically appropriate.
- Comprehensive assessment: A thorough assessment of pre-existing conditions, cognitive function, and pre-fracture mobility is crucial for developing personalized rehabilitation plans.
- Addressing delays in surgery: Healthcare systems should strive to minimize delays between hospital admission and surgery to improve patient outcomes. This is often a challenge in the U.S. due to factors like insurance approvals and operating room availability.
- Patient education: educating patients and their families about the importance of early ambulation and the factors that can influence recovery can empower them to actively participate in the rehabilitation process.
Recent Advances in Hip Fracture Care
Several recent developments are further improving hip fracture care in the U.S.:
- improved surgical techniques: Minimally invasive surgical techniques are becoming more common,leading to less pain and faster recovery times.
- Enhanced pain management: Advances in pain management, including the use of regional anesthesia and multimodal analgesia, are helping patients tolerate early mobilization.
- Telehealth and remote monitoring: Telehealth and remote monitoring technologies are being used to provide ongoing support and guidance to patients after discharge, helping them maintain their mobility and independence.
Addressing Potential Concerns
while early ambulation is generally beneficial,some healthcare providers might potentially be hesitant to implement it due to concerns about patient safety and potential complications. However, studies have shown that early ambulation is safe and effective when implemented under appropriate medical supervision.careful patient selection, adequate pain management, and close monitoring are essential to minimize risks.
Another potential concern is the cost of implementing early ambulation protocols. Though, the long-term benefits of improved mobility and reduced hospital stays can outweigh the initial costs.
Conclusion: A Path to Improved Recovery
Early ambulation after hip fracture surgery is a critical factor in helping patients regain their walking independence.By prioritizing early mobilization, conducting comprehensive assessments, and addressing delays in surgery, U.S. healthcare systems can significantly improve outcomes for hip fracture patients, enabling them to live more active and independent lives. As the population ages,these improvements will become even more crucial in maintaining the health and well-being of older Americans.
Early Ambulation After Hip Fracture Surgery Linked to Improved Walking Independence
By Archyde News Journalist
The Importance of Early Mobility
For older adults in the U.S. recovering from hip fracture surgery, regaining the ability to walk independently is a major goal. A recent study investigated the impact of early ambulation – that is, starting to walk soon after surgery – on achieving this goal.
The study focused on understanding whether initiating walking exercises in the immediate postoperative period could significantly improve a patient’s chances of walking independently by the time they are discharged from the hospital, and also one week postoperatively. This is particularly relevant in the American healthcare context, where hospitals are continuously seeking to optimize patient recovery and reduce readmission rates.
Study Design and Methodology
The research team employed rigorous statistical methods to analyze the data. Here’s a breakdown of their approach:
- Univariate Logistic Regression: This initial analysis assessed the basic relationship between early ambulation and independent walking at discharge, without accounting for other influencing factors.
- Multivariate Logistic Regression (Model 1): This more complex analysis aimed to determine if early ambulation affected independent walking at 1 week postoperatively and at discharge, while controlling for confounding variables.
- Generalized Linear Mixed Model (Model 2): Similar to Model 1, this model further accounted for inter-hospital variability, recognizing that different hospitals might have varying protocols and resources that could impact patient outcomes.
To account for the numerous factors that could influence a patient’s likelihood of being assigned to the early ambulation (EA) or late ambulation (LA) group, the researchers used a technique called propensity score matching. This approach effectively condenses all potential confounding factors into a single score, which is then used to adjust the analysis, ensuring a fairer comparison between the two groups.
According to Biondi-Zoccai et al. (2011) in “Are propensity scores really superior to standard multivariable analysis?”, propensity scores can offer a robust method for reducing bias in observational studies contemp. Clin. Trials 32, 731–740 (2011).
Missing data, which can be a problem in many clinical studies, was handled carefully. The researchers chose to exclude missing values, recognizing that they represented a small fraction of the overall dataset.
Subgroup Analyses: Understanding Specific Patient Groups
To gain a deeper understanding of the impact of early ambulation,the researchers conducted several subgroup analyses:
- Stratified Subgroup analysis: This analysis examined the relationship between early ambulation and independent walking at discharge across different patient subgroups,based on characteristics like age,pre-fracture walking status,cognitive impairment,fracture type,and comorbidities (co-existing medical conditions).
- Gait training Subgroup: A separate analysis focused specifically on patients who were able to participate in gait training during their hospitalization.
- Postoperative ambulation Timing: This analysis evaluated outcomes based on different postoperative ambulation timings (days 1-2,3-4,and 5-6).
These subgroup analyses are particularly important because they can help doctors tailor rehabilitation plans to individual patients. For example,an 80-year-old patient with pre-existing arthritis might benefit from a different approach than a 65-year-old who was highly active before their fracture.
To address the potential impact of missing data on postoperative walking timing and recovery, the researchers performed logistic regression analysis utilizing multiple imputation methods, as outlined by Marshall, Altman, Holder, & Royston (2009) in BMC Med. Res. Methodol. Combining estimates of interest in prognostic modelling studies after multiple imputation: current practice and guidelines.
Furthermore, to assess the influence of unknown confounders on the relationship between early postoperative ambulation and independent walking, the researchers calculated E-values, as described by vanderweele, T. J. & Ding, P. (2017) in Ann. Intern. Med. Sensitivity analysis in observational research: Introducing the E-value.
Statistical software
R, version 4.3.2 (https://www.r-project.org) was used for statistical analysis.
Practical Applications and Implications for U.S. Healthcare
The findings of this study have significant implications for how hip fracture recovery is approached in the United States:
- Early Ambulation Protocols: Hospitals may want to consider implementing or strengthening early ambulation protocols for hip fracture patients. This could involve training staff, allocating resources for physical therapy, and ensuring that patients are medically stable enough to begin walking soon after surgery.
- Personalized Rehabilitation: The subgroup analyses highlight the importance of tailoring rehabilitation plans to individual patient needs. Factors like age, pre-existing conditions, and cognitive function should all be taken into account.
- Reducing Readmissions: By promoting independent walking, hospitals can potentially reduce readmission rates, which are a major concern for the Centers for Medicare & Medicaid Services (CMS).
- Cost-Effectiveness: While early ambulation requires an initial investment of resources, it could ultimately be cost-effective by reducing the length of hospital stays and the need for long-term care.
Potential Counterarguments and Considerations
While the study suggests a strong link between early ambulation and improved walking independence, it’s critically important to acknowledge potential counterarguments:
- Patient Safety: Some doctors might potentially be hesitant to implement early ambulation protocols due to concerns about patient safety, particularly for those with complex medical conditions. Careful patient selection and monitoring are essential.
- Resource Constraints: Many hospitals in the U.S., particularly those in rural areas or serving underserved populations, face resource constraints that could make it arduous to implement comprehensive early ambulation programs.
- Generalizability: The study’s findings may not be fully generalizable to all populations. Further research is needed to confirm these results in diverse patient groups.
Recent Developments and Future Research
The field of hip fracture rehabilitation is constantly evolving.recent developments include:
- Use of Technology: Wearable sensors and virtual reality (VR) are being used to track patient progress and provide personalized feedback during rehabilitation.
- Focus on Prehabilitation: Some hospitals are starting to focus on “prehabilitation” – preparing patients for surgery and recovery before the procedure even takes place. This can involve exercises, nutrition counseling, and education.
- Telehealth: Telehealth is being used to provide remote monitoring and support to patients after they are discharged from the hospital.
Future research should focus on:
- Long-term Outcomes: Studies are needed to assess the long-term impact of early ambulation on patient function, quality of life, and mortality.
- Cost-Effectiveness Analyses: More research is needed to determine the cost-effectiveness of different rehabilitation strategies.
- Implementation Strategies: Studies are needed to identify the best ways to implement early ambulation programs in different healthcare settings.
]
Interview: Dr. Evelyn reed on Early Ambulation After Hip Fracture Surgery
Introduction
Welcome to Archyde News. Today, we have Dr. Evelyn Reed, a leading geriatric rehabilitation specialist, wiht us to discuss the important topic of early ambulation following hip fracture surgery. Dr. Reed, thank you for joining us.
Dr. Reed: Thank you for having me. It’s a pleasure to be here.
The Meaning of Early Ambulation
Archyde News: Dr. Reed, can you explain why early ambulation is so critically important for patients recovering from hip fracture surgery? We’ve seen recent studies, including those from japan, highlighted in our articles.
Dr. Reed: Certainly. Early ambulation, in simple terms, is getting patients moving as soon as medically feasible after hip fracture surgery. The benefits are multifaceted.Firstly,it helps prevent complications like pneumonia and blood clots,which are serious risks for elderly patients after surgery. Secondly, it promotes faster recovery of walking ability and overall function.Independent walking is a key goal, and getting patients up and moving early substantially increases their chances of achieving that.
Key Findings from the Japanese Study
Archyde News: The Japanese study we referenced appears to support this. What were some of the key findings that you found most impactful?
Dr. Reed: The study provided strong evidence that patients who started walking within the first two days after surgery had a higher likelihood of independent walking at discharge. It further underscored the need to reevaluate existing post-operative protocols and promote a focus on getting patients mobile as early as possible. The benefits were clear.
Implications for U.S. Healthcare
Archyde News: How can these findings translate into practical improvements in U.S. healthcare settings, particularly given the high number of hip fracture cases?
Dr. Reed: Several ways. First, hospitals need to review and possibly revise their established post-operative rehabilitation protocols to encourage and support the early mobilization of patients. This would require a team effort and include, and is not limited to, physical therapists and nursing staff. Next, patient education is crucial. Patients and their families has to understand the benefits of early ambulation and their importance in the recovery process. Healthcare facilities may need to put more resources into support systems that are centered around these newer recovery protocols.
Addressing Potential Concerns
Archyde News: There could be concerns regarding the immediate implementation of these findings. What challenges might healthcare providers face, and how can they be addressed?
Dr. Reed: One primary concern is patient safety. Not all patients are immediately ready for early ambulation, particularly those with other medical conditions. It’s very important that healthcare professionals carefully assess each patient. Pain management is another factor. Ensuring patients are comfortable is key. Healthcare facilities must also commit to training and have the proper resources. Collaboration between surgeons, rehabilitation specialists, and nurses is essential to ensure a safe and effective ambulation program.
Future Research and Developments
Archyde News: Are there any emerging areas for research or new technologies that could further enhance hip fracture recovery?
Dr. Reed: Absolutely. Researchers are exploring the use of wearable sensors and virtual reality (VR) to help track patient progress and deliver personalized feedback, which is quite exciting. Prehabilitation – preparing patients before surgery – is also gaining traction. This means pre-surgery tailored exercise, education, and nutritional planning. And telehealth might allow for remote monitoring and support. These elements are poised to shape the trajectory of hip fracture care in the coming years.
Call To Action
Archyde News: Dr. Reed, if our readers could take away one key message, what would it be?
Dr. Reed: Prioritize early, safe ambulation following hip fracture surgery. This is not only about helping patients walk. It’s about improving their overall quality of life, and independence. The evidence is there.let us make hip fracture recovery a success.
Reader Engagement
Archyde News: Thank you, Dr. Reed, for such insightful thoughts. We are keen to hear from our readers. What challenges have you, or your loved ones, experienced in hip fracture recovery? Share your insights and experiences in the comments below.
Conclusion
Archyde News: Thank you for tuning in to Archyde news. We hope this discussion has provided valuable insights into improving hip fracture recovery.