This case highlights how targeted pharmacological interventions can have unintended consequences.
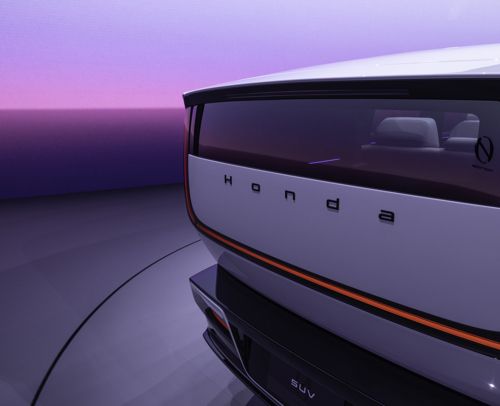
FIGURE 1. A patient with psoriasis who was treated with secukinumab subsequently developed atopic dermatitis. A. Diffuse erythema and edema of the lower extremities. B, Diffuse erythema and scaling of the back.
And case clinician in literature narrates the finding of a patient diagnosed with psoriasisand under a controlled condition, which developed a erythroderma severe refractory drug-induced medicine biological and puts in the inkwell that, sometimes, targeted therapies might have unintended consequences.
Although they emphasize that more studies are needed to continue describing the mechanisms of action of this type of drug, they maintain that in this 39-year-old man with a history of psoriasis who was admitted to hospital for treatment of severe erythroderma, which is defined as a inflammatory skin syndrome characterized by scaling and erythema over more than 90 percent of the body surface.
It was reported that four years earlier he had started treatment with secukinumab -monoclonal drug- for psoriasis, with an excellent clinical response. Likewise, it was suspended following 2 years of treatment due to insurance coverage problems and he controlled his disease only with topical corticosteroids.
It is added that he resumed secukinumab 10 months before admission due to a flare of psoriasis. Shortly therefollowing, she developed severe exfoliative erythroderma—also called generalized exfoliative dermatitis and a severe inflammation of the total surface of the skin—that did not respond to corticosteroids, etanercept, methotrexate, or ustekinumab.
In this case, the medications known as corticosteroids are drugs that act by regulating the immune system response and decreasing cellular production of substances that cause intestinal inflammation.
At initial presentation, physical examination revealed erythema diffuse and scaling with edema associated on the face, trunk, and extremities. A right arm biopsy of the patient showed a superficial inflammatory infiltrate composed of scattered lymphocytes, histiocytes and eosinophils, compatible with spongiotic dermatitis. The administration of cyclosporine 225 mg twice a day and topical corticosteroids was started, according to the case report.
Spongiotic dermatitis is a term pathologists use to describe a pattern of skin injury caused by inflammation. Meanwhile, cyclosporine and cyclosporine belong to a class of drugs called immunosuppressants. They act by decreasing the immune system activity.
Four months following initial hospitalizationall psoriasis medications were discontinued, and the patient was started on dupilumab every 2 weeks and once reduction of oral prednisone for 8 weeks. Is combination produced a marked improvement symptoms and resolution of peripheral eosinophilia.
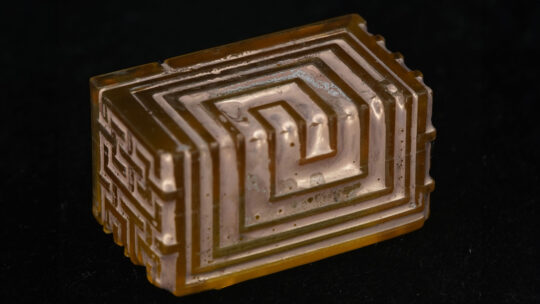
Histopathology revealed new psoriatic lesions following treatment of atopic dermatitis with dupilumab (H&E, original magnification ×20).
However, several months following disease remission, worsening erythema and pruritus began to appear on the trunk and extremities, followed by the appearance of new psoriatic lesions with a biopsy consistent with psoriasis. The patient continued with dupilumab -a biological drug-, but cyclosporine was added.
The patient stopped taking dupilumab due to injection site discomfort, and has been slowly weaning off oral cyclosporine, with 1-2 eczematous plaques remaining and 1-2 psoriatic plaques treated with topical corticosteroids.
Precisely this case highlights how pharmacological interventions targeting specific immune pathways, such as the TH1/TH2 axis (inflammatory cytokines) can have unintended consequences.
Regarding the TH1, TH2 and TH17 cells, it is known that in addition to being collaborators, they have suppressive functions of the other responses, since they are mutually antagonistic.
“We present an unusual case of secukinumab-induced exfoliative dermatitis in a patient with psoriasis that, although resolved following several months of treatment with dupilumab and a tapering dose of prednisone, subsequently developed recurrence of psoriatic lesions with continued use of dupilumab. , which was finally suspended by the patient despite adequate control of the disease”, highlights the case report, which also maintains that more studies are needed aimed at a better understanding of the immune mechanism of TH1/TH2 inflammatory cytokines.
Access the case here.