What is diabetes? Type 1 Diabetes and Type 2 Diabetes
Diabetes mellitus is a type of metabolic disease caused by insufficient or abnormal insulin secretion, and causes an increase in blood glucose concentration or excretion of glucose in urine due to a lack of insulin. Diabetes is divided into type 1 diabetes, commonly called childhood diabetes, and type 2 diabetes due to obesity.
In type 1 diabetes, if the insulin-producing cells (beta cells) of the pancreas are congenitally absent, the insulin-producing cells are attacked by autoimmune cells (type 1a) or some or all of them are destroyed due to an external cause (type 1b). It is a disease that occurs when you cannot produce insulin (insulin deficiency) and lose the ability to manage blood sugar. Diabetics who have lost the ability to control their blood sugar may have their blood sugar drop below normal (acute hypoglycemia). People with type 1 diabetes are very difficult to manage, and their daily life itself is severely limited. Currently, injection treatment is possible, and clinical trials such as pills and patches are in progress.
Type 2 diabetes is a disease in which beta cells secrete a sufficient amount of insulin, but the cells do not recognize it (insulin resistance), resulting in hyperglycemia. It is a disease that can be treated with medications and can be treated with exercise and diet control. Although the causes are very diverse, it is mainly identified as obesity caused by a westernized high-calorie diet. Diabetes mellitus progresses as the level of free fatty acids in the blood increases due to obesity and glucose uptake in the muscles decreases, resulting in insulin resistance and at the same time producing more glucose in the liver.
Why Diabetes Is Dangerous
Diabetes mellitus is dangerous because most patients have no symptoms. In relatively weak hyperglycemia, the more blood sugar rises, the more water you drink, the more you urinate, and the more weight you lose. In addition, when high blood sugar is maintained for a relatively long period of time, various complications occur and kidney or cardiovascular disease increases. However, since symptoms do not appear significantly until complications develop, few people are aware of the disease until the examination. Therefore, it is very dangerous to control blood sugar only with symptoms you feel yourself, and you must be able to measure your blood sugar accurately.
The key to diabetes treatment – pancreatic islet cells
Insulin required for blood sugar control is produced in the pancreatic islet cells (or pancreatic islet cells or islet cells – mainly composed of beta cells and alpha cells) in the pancreas. It is being studied intensively in treatment. Currently, treatment is focused on transplantation of pancreatic islet cells from brain-dead donors, but the shortage of donors is a problem, and the production of pancreatic islet cells by inducing differentiation from pluripotent stem cells has not yet reached the stage of medical application. am.
Diabetes treatment potential through pancreatic islet cell proliferation – MYCL gene expression
On February 10, the Research Center for Experimental Medicine and Systems Biology, Faculty of Stem Cell Pathology, University of Tokyo, led by Prof.Nature Metabolism) was published.
Overview of the study of the potential for treating diabetes through pancreatic islet cell proliferation © Michitada Hirano et al. 2022
The research team first noted that pancreatic cells before and following birth have the ability to self-proliferate. They also found that the expression of a gene called ‘MYCL’ is very important for self-renewal ability. Next, the research team succeeded in proliferating the cells through reprogramming following strongly activating the gene called MYCL in pancreatic islet cells collected from mice. When the proliferated cells were administered to diabetic old rats, insulin secretion returned to near normal levels, and it was confirmed that blood sugar also dropped to normal levels. This is a study that showed that it is possible to treat diabetes in mice through ‘pancreatic islet cells with high functionality’ as a result of the successful amplification of mature pancreatic islet cells, which has been considered impossible until now.
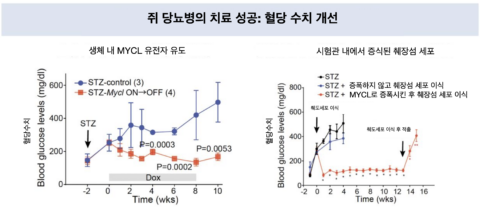
Improving blood glucose levels in diabetic rats (left). Observation of blood glucose levels following administration of STZ (a drug that destroys pancreatic beta cells) with pancreatic islet cells proliferated in vitro (right) © Michitada Hirano et al. 2022
Human pancreatic islet cells can be proliferated in the same way.
The biggest achievement of the research team is that they found that it was possible to induce autoproliferation of mature pancreatic islet cells in vitro, and also confirmed that human pancreatic islet cells can be proliferated in the same way. This is good news for patients with diabetes, who are considered a chronic disease and that there is no cure. Professor Yasuhiro Yamada’s research team said that the above results are still in the rat experimental stage, but they are paying attention as a research result that can completely change the paradigm of diabetes treatment. The research team announced that they are planning a clinical trial within five years, such as proliferating pancreatic islet cells and transplanting them into patients with severe diabetes, and that they will develop a new treatment. In addition, various applied studies are expected for the development of cell regenerative medicine, such as cell transplantation to return pancreatic islet cells amplified in vitro by the MYCL gene back into the body or the development of in vivo pancreatic islet cell amplification technology by MYCL gene therapy. .
(16)
