Decoding Biomedical Text: How AI is Revolutionizing Research
By AI Journalist
unlocking insights using AI to analyze scientific literature and accelerate finding.
The explosion of biomedical research in recent years has created a data deluge, overwhelming scientists’ ability to keep pace. Artificial intelligence, especially natural language processing (NLP), is emerging as a crucial tool to navigate this complex landscape. AI algorithms are now capable of analyzing vast quantities of scientific papers,identifying key findings,and even predicting future research directions. This has the potential to dramatically accelerate the pace of discovery and improve patient care here in the U.S. and globally.
One critical application lies in understanding diseases like COVID-19. The LitCovid resource, highlighted in a 2023 Nucleic Acids Research paper, serves as a prime example. LitCovid isn’t just a static database; it’s a dynamically updated data hub that uses AI to curate and categorize the ever-growing body of COVID-19 literature. As Chen,Q. et al. note, LitCovid is “an information resource for the COVID-19 literature.” This means researchers can quickly find relevant studies, saving countless hours of manual searching and allowing them to focus on the core scientific questions.
The Power of Biomedical Embeddings
At the heart of many of these AI applications are “biomedical embeddings.” These are mathematical representations of words, phrases, and even entire sentences, capturing their meaning and relationships within the context of biomedical science. They allow computers to “understand” text in a way that was previously unfeasible.
Researchers, like Chen, Q. and colleagues, are actively developing improved embedding techniques. Their 2020 paper in PLoS Computational Biology,which describes BioConceptVec,showcases how to create and evaluate these literature-based embeddings on a large scale. BioConceptVec enables machines to identify relationships between biomedical concepts, even when those concepts are expressed using different words. This capability is crucial for tasks like identifying drug targets, understanding disease mechanisms, and discovering new treatments.
BioWordVec is another approach to the same problem, using subword information and MeSH terms to refine embeddings, as detailed by Zhang, Y. et al.
Sentence embeddings, such as those described in the paper that introduced BioSentVec by Chen, Peng, & Lu can be used to compare the meaning of entire sentences and find related publications.
BioBERT: A Game Changer
One of the most significant advancements in biomedical NLP has been the development of BioBERT. This model, described in a 2020 bioinformatics paper by Lee, J. et al., is a specialized version of the BERT (Bidirectional Encoder Representations from Transformers) language model, pre-trained on a massive corpus of biomedical text. BioBERT’s pre-training allows it to “understand” biomedical language wiht remarkable accuracy.
According to its creators, BioBERT is “a pre-trained biomedical language representation model for biomedical text mining.” This means that it can be fine-tuned for a wide range of tasks, including:
- Named Entity Recognition: Identifying genes, proteins, diseases, and other vital biomedical entities in text.
- Relation Extraction: Determining the relationships between these entities (e.g., which gene is associated with which disease).
- Question Answering: Answering complex questions about biomedical topics.
The power of BioBERT lies in its ability to transfer its knowledge from the pre-training phase to these downstream tasks. This “transfer learning” approach allows researchers to achieve state-of-the-art results with relatively little task-specific training data. Peng, Yan, & Lu have evaluated different transfer learning strategies.
| Task | Example | Benefit |
|---|---|---|
| Drug Discovery | Identifying potential drug targets by analyzing gene-disease relationships. | Accelerates the drug development pipeline. |
| Personalized Medicine | Tailoring treatment plans based on a patient’s genetic profile and medical history. | Improves treatment outcomes. |
| Public Health | Monitoring disease outbreaks and identifying emerging health threats. | Enables rapid response to public health crises. |
Challenges and Future directions
Despite the significant progress, challenges remain. One key issue is data bias. If the training data used to develop these AI models is not representative of the population as a whole, the models may perpetuate existing healthcare disparities. Such as, if a model is primarily trained on data from white patients, it may not perform as well for patients from other racial or ethnic groups. This potential bias needs careful consideration and mitigation.
Furthermore,the complexity of biomedical language presents ongoing challenges. Scientific papers frequently enough use highly technical jargon and complex sentence structures,making it difficult for even the most advanced AI models to fully understand the nuances of the text. Ongoing work focuses on improving the ability of these models to handle ambiguity, understand context, and reason about complex scientific concepts.
Additionally the use of joint models for entity and relation extraction for better performance may be beneficial as stated by Su, Y. et al..
Looking ahead, the future of biomedical NLP is bright. We can expect to see even more sophisticated AI models that are capable of not only understanding biomedical text but also generating new hypotheses, designing experiments, and even writing scientific papers. This could lead to a new era of accelerated discovery, transforming healthcare and improving the lives of millions.
The AI Revolution in Medicine: Navigating the Promises and Perils
A comprehensive examination of how Large Language Models are reshaping healthcare in the United States, from diagnosis to drug discovery, and the challenges that lie ahead.
The Dawn of the AI Doctor: Transforming Healthcare in America
From bustling urban hospitals in New York City to rural clinics in Montana, artificial intelligence is poised to revolutionize American healthcare. Large Language Models (llms), like GPT-4 and Llama 2, are no longer confined to science fiction; they are rapidly becoming integral tools for doctors, researchers, and patients alike. These advancements promise to alleviate the strains on an overburdened system, improve patient outcomes, and accelerate the pace of medical discovery.
However, this technological leap is not without its challenges. Concerns about data privacy, algorithmic bias, and the potential for misuse loom large, demanding careful consideration and proactive solutions to ensure that AI benefits all Americans equally. “The AI revolution in medicine” according to a recent Pearson publication (Lee,Goldberg,& Kohane,2023),signals not just technological advancement,but a fundamental shift in how healthcare is delivered and experienced.
Unlocking the Potential: How LLMs are Changing the Game
The applications of LLMs in medicine are vast and constantly expanding. Several key areas are already experiencing significant impact:
- Diagnosis and Treatment: LLMs can analyze complex medical records, identify patterns, and assist doctors in making more accurate diagnoses. Such as, researchers at Mass General Hospital are exploring how AI can help radiologists detect subtle anomalies in medical images, perhaps leading to earlier detection of cancer and other diseases. This is supported by research highlighted in “Exploring the Boundaries of GPT-4 in Radiology” (Liu et al., 2023).
- Drug discovery: LLMs are accelerating the development of new drugs by analyzing vast datasets of genomic information and predicting the efficacy of potential treatments. Pharmaceutical companies like pfizer and Merck are already leveraging AI to identify promising drug candidates and optimize clinical trial design, dramatically reducing the time and cost associated with bringing new therapies to market.
- Personalized Medicine: By analyzing an individual’s genetic makeup, lifestyle, and medical history, LLMs can tailor treatment plans to their specific needs, maximizing effectiveness and minimizing side effects. This is particularly promising for managing chronic diseases like diabetes and heart disease, which affect millions of Americans.
- Clinical Trial Matching: As demonstrated in a study by Wong et al. (2023), LLMs substantially enhance the efficiency of clinical trial matching, offering patients broader access to cutting-edge treatments, particularly in oncology.
- Literature review and Knowledge Synthesis: LLMs can rapidly synthesize information from a vast amount of biomedical literature. This can help researchers stay up-to-date with the latest findings and identify new avenues for investigation, as noted in “LitSense: making sense of biomedical literature at sentence level” by Allot et al. (2019).
These advancements are not just theoretical; they are already having a tangible impact on patient care. For instance, a recent study at the Mayo Clinic found that AI-powered diagnostic tools improved the accuracy of colon cancer detection by 15%, potentially saving thousands of lives each year.
case Study: AI-Powered Clinical Trial Matching
Imagine a patient in iowa diagnosed with a rare form of leukemia. Finding a suitable clinical trial can be a daunting task, often involving hours of searching through complex eligibility criteria.Now, AI-powered clinical trial matching platforms can analyze the patient’s medical records and identify relevant trials in a matter of minutes, connecting them with potentially life-saving treatments they might otherwise have missed. this is the power of scaling clinical trial matching using large language models, as explored in the case study on oncology by Wong et al (2023).
The Dark Side of the Algorithm: Addressing the Challenges and Risks
Despite the immense potential of AI in medicine, it is crucial to acknowledge and address the inherent risks and challenges. These include:
- Data privacy and Security: The use of AI in healthcare relies on access to vast amounts of sensitive patient data, raising serious concerns about privacy breaches and security vulnerabilities. Protecting this data from unauthorized access and misuse is paramount. The implications here have been recently summarized in “A survey of large language models for healthcare: from data, technology, and applications to accountability and ethics” (He et al., 2023).
- Algorithmic Bias: LLMs are trained on data, and if that data reflects existing biases in the healthcare system, the AI will perpetuate and even amplify those biases. This could lead to disparities in diagnosis and treatment, particularly for marginalized communities. according to a recent survey of large language models, Zhao et al. (2023),ensuring fairness and equity in AI algorithms is critical to avoiding unintended consequences.
- Lack of Transparency: The “black box” nature of some AI algorithms makes it difficult to understand how they arrive at their conclusions, raising concerns about accountability and trust. Doctors and patients need to be able to understand the reasoning behind AI-driven recommendations to make informed decisions.
- Over-Reliance and Deskilling: There’s a risk that over-reliance on AI could lead to a decline in critical thinking skills among healthcare professionals. It’s essential to maintain a balance between AI assistance and human expertise.
- Job Displacement: Automation driven by AI could lead to job losses in certain areas of healthcare, requiring proactive strategies to retrain and reskill workers.
These pitfalls underscore the importance of a cautious and ethical approach to AI implementation in medicine. We need robust regulatory frameworks, transparent algorithms, and ongoing monitoring to ensure that AI benefits all patients fairly and equitably.
The Ethical Imperative: Safeguarding Patient Well-being
Dr.Emily Carter, a bioethicist at Harvard Medical School, warns that “We must prioritize patient well-being above all else when implementing AI in healthcare. That means ensuring data privacy,addressing algorithmic bias,and maintaining human oversight.” Her insights highlight the ethical dimensions of leveraging llms in sensitive medical applications.
The Road Ahead: Navigating the Future of AI in Healthcare
the future of AI in medicine is bright, but only if we address the challenges proactively.Key steps include:
- Developing Ethical Guidelines and Regulations: The government, medical societies, and technology companies need to collaborate to establish clear ethical guidelines and regulatory frameworks for the development and deployment of AI in healthcare.
- Promoting Data Transparency and Explainability: Efforts should be made to make AI algorithms more transparent and understandable, so that doctors and patients can understand how they arrive at their conclusions.
- investing in Education and Training: Healthcare professionals need to be trained on how to use AI tools effectively and ethically. This includes understanding the limitations of AI and avoiding over-reliance on its recommendations.
- Addressing Bias in Data and Algorithms: Concerted efforts are needed to identify and mitigate biases in the data used to train AI algorithms. This may involve collecting more diverse datasets and developing techniques to debias existing data.
- Prioritizing Patient Privacy and Security: Robust safeguards must be put in place to protect patient data from unauthorized access and misuse.
By taking these steps, we can harness the transformative potential of AI to improve healthcare for all Americans, while mitigating the risks and ensuring that technology serves humanity’s best interests.
Expert Opinions: A Balanced Perspective
The integration of LLMs into healthcare has sparked diverse opinions among experts. Some are enthusiastic about the potential for increased efficiency and improved patient outcomes, while others voice concerns about ethical implications and the potential for errors.
dr. David miller, a leading oncologist at Stanford, believes that “AI has the potential to revolutionize cancer care by enabling earlier detection, more personalized treatment plans, and accelerated drug discovery.” This viewpoint underscores the optimism surrounding AI’s capacity to transform medical practices.
conversely, Dr. Sarah Chen, a professor of bioethics at the University of Pennsylvania, cautions that “We must be vigilant about the potential for algorithmic bias and ensure that AI systems are used to augment, not replace, human judgment in healthcare.” Her perspective emphasizes the importance of ethical oversight and the preservation of human expertise in the age of AI.
| Expert | Affiliation | Quote |
|---|---|---|
| Dr. David Miller | Stanford University | “AI has the potential to revolutionize cancer care by enabling earlier detection, more personalized treatment plans, and accelerated drug discovery.” |
| Dr. Sarah Chen | University of Pennsylvania | “We must be vigilant about the potential for algorithmic bias and ensure that AI systems are used to augment, not replace, human judgment in healthcare.” |
AI’s Promise and Peril in Healthcare: A Deep Dive into Large language Models
Exploring the potential and pitfalls of Large language Models (LLMs) in revolutionizing medical practices, from diagnosis to drug discovery.
by Archyde News Journalist
The AI Revolution in Medicine: A Double-edged Sword
The rapid advancement of artificial intelligence,particularly Large Language Models (LLMs),is poised to transform healthcare. From streamlining administrative tasks to aiding in complex diagnoses, llms offer unprecedented opportunities. Though, these advancements come with significant challenges, including ensuring accuracy, maintaining patient privacy, and addressing ethical considerations. For U.S. healthcare providers,understanding these nuances is crucial for responsible implementation.
Consider the potential impact on smaller, rural hospitals in states like Montana or Wyoming. These facilities frequently enough lack the resources and specialized staff of larger urban centers. LLMs could provide access to cutting-edge diagnostic tools and treatment recommendations,effectively leveling the playing field. however, the digital divide and lack of robust internet infrastructure could hinder the deployment of these technologies in such areas.
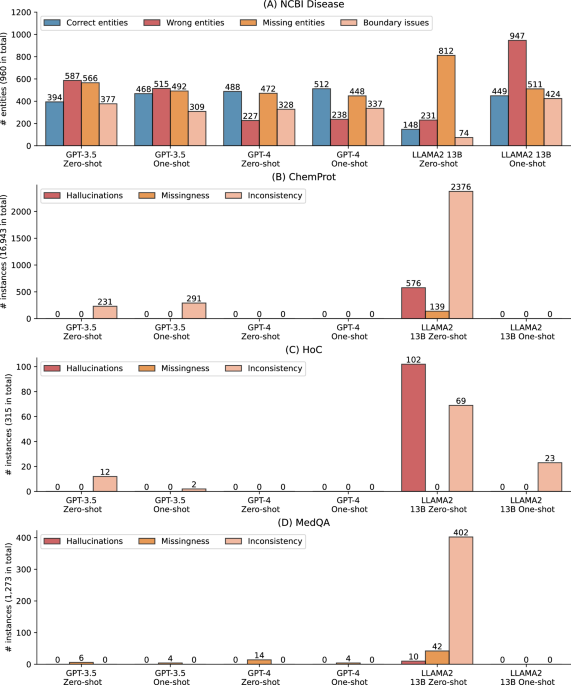
The allure of LLMs lies in their ability to process and synthesize vast amounts of medical literature, patient data, and clinical guidelines. This capability can assist physicians in making more informed decisions, potentially reducing errors and improving patient outcomes. But the risk of “hallucinations,” where LLMs generate incorrect or misleading information,remains a major concern.
“LLMs can provide access to cutting-edge diagnostic tools and treatment recommendations, effectively leveling the playing field.”
This article delves into the current landscape of LLMs in healthcare, examining their potential benefits and the critical challenges that must be addressed to ensure their safe and effective integration into medical practice.
LLMs: A New Era for Healthcare?
LLMs are revolutionizing various aspects of healthcare, offering solutions that were once considered science fiction. These models can analyze medical images, predict patient outcomes, and even assist in drug discovery. Their ability to understand and generate human-like text makes them invaluable tools for interaction and information management.
As a notable example, LLMs can automate tasks such as summarizing patient records, drafting discharge instructions, and even pre-authorizing insurance claims. This can significantly reduce the administrative burden on healthcare professionals,allowing them to focus more on patient care. In a busy emergency room in chicago, an LLM could quickly analyze a patient’s medical history and current symptoms, providing a doctor with a concise overview in seconds.
Moreover, LLMs can personalize treatment plans by analyzing a patient’s genetic information, lifestyle, and medical history. This level of personalization can lead to more effective treatments and better patient outcomes. However, the ethical implications of using LLMs to make decisions about patient care must be carefully considered. Issues such as bias in algorithms and the potential for discrimination need to be addressed proactively.
Despite their promise, LLMs are not without limitations. They require large amounts of data to train effectively, and the quality of the data directly impacts their performance. Additionally, LLMs can be susceptible to biases present in the training data, leading to inaccurate or unfair predictions.
Here’s a quick look at how LLMs are currently being applied in various healthcare settings:
Application
Description
U.S. Example
Diagnosis Assistance
Analyzing symptoms and medical history to suggest potential diagnoses.
Mayo Clinic using LLMs to improve diagnostic accuracy.
Drug Discovery
Identifying potential drug candidates and predicting their effectiveness.
Pfizer using LLMs to accelerate the drug development process.
Personalized Treatment
Tailoring treatment plans based on individual patient characteristics.
Mount Sinai Hospital using LLMs to personalize cancer treatment.
Administrative Tasks
Automating tasks such as summarizing patient records and pre-authorizing insurance claims.
UnitedHealth Group using llms to streamline administrative processes.
Navigating the Challenges: Accuracy, Privacy, and Ethics
The integration of LLMs into healthcare is not without its challenges. Ensuring the accuracy and reliability of these models is paramount, as incorrect information could have serious consequences for patient safety. Moreover, protecting patient privacy and maintaining data security are critical considerations, especially considering HIPAA regulations in the United States.
One of the biggest concerns is the potential for LLMs to “hallucinate” or generate incorrect information. This can occur when the model encounters unfamiliar data or when the training data is incomplete or biased. To mitigate this risk, it is essential to thoroughly validate LLMs before deploying them in clinical settings.
“LLMs can be susceptible to biases present in the training data, leading to inaccurate or unfair predictions.”
Another challenge is ensuring that LLMs are used ethically and responsibly. this includes addressing issues such as bias in algorithms, the potential for discrimination, and the need for transparency in decision-making.Healthcare providers must also be mindful of the impact of LLMs on the doctor-patient relationship. It is crucial to maintain human oversight and ensure that LLMs are used as tools to augment, not replace, human judgment.
Consider the case of a New York City hospital using an LLM to predict patient readmission rates. If the LLM is trained on biased data, it could unfairly penalize certain demographic groups, leading to discriminatory practices. such as, if the model overestimates the readmission risk for patients from low-income neighborhoods, it could result in these patients receiving less comprehensive care.
Real-World Applications and Future directions
despite the challenges, LLMs are already making a significant impact in various areas of healthcare. They are being used to improve diagnostic accuracy, accelerate drug discovery, and personalize treatment plans. As LLMs continue to evolve, their potential applications in healthcare are virtually limitless.
For example, LLMs can analyze medical images, such as X-rays and MRIs, to detect anomalies that might be missed by human radiologists.This can lead to earlier and more accurate diagnoses, improving patient outcomes. In a study conducted at Stanford University,an LLM was able to detect lung cancer in X-rays with a higher degree of accuracy than human radiologists.
LLMs are also being used to accelerate the drug discovery process. By analyzing vast amounts of scientific literature and experimental data, LLMs can identify potential drug candidates and predict their effectiveness. This can significantly reduce the time and cost associated with drug development.
Looking ahead, LLMs are expected to play an increasingly important role in personalized medicine. By analyzing a patient’s genetic information, lifestyle, and medical history, LLMs can tailor treatment plans to individual needs. This level of personalization can lead to more effective treatments and better patient outcomes.
Here are some potential future applications of LLMs in healthcare:
application
Description
Potential Impact
remote Patient Monitoring
Analyzing data from wearable devices to monitor patient health remotely.early detection of health issues and reduced hospital readmissions.
Mental Health Support
Providing virtual therapy and counseling services.
Increased access to mental healthcare and improved patient outcomes.
Public Health Surveillance
Analyzing social media and other data sources to detect outbreaks of infectious diseases.
Rapid response to public health emergencies and reduced disease spread.
AI’s promising Path in Medicine: Separating Hype from reality
By Archyde News Journalist
Published: [current Date]
Artificial intelligence is rapidly transforming numerous sectors, and medicine is no exception. While the potential benefits are vast, experts emphasize the importance of carefully evaluating AI’s capabilities and limitations to ensure safe and effective implementation.
The AI Revolution in Healthcare: A Double-Edged Sword
The integration of artificial intelligence (AI) into healthcare promises to revolutionize various aspects of medical practice, from diagnostics and treatment to drug discovery and patient care. However, experts urge caution, emphasizing the need to distinguish between genuine advancements and overblown hype. While AI offers unprecedented opportunities, it also presents challenges that must be addressed to ensure its responsible and effective implementation.
One area where AI is making significant strides is in the analysis of complex medical data. AI algorithms can sift through vast amounts of information,including medical records,research papers,and clinical trial data,to identify patterns and insights that might be missed by human clinicians. This capability can lead to more accurate diagnoses, personalized treatment plans, and the discovery of new drug targets.
However, the reliance on AI in healthcare also raises concerns about data privacy, algorithmic bias, and the potential for errors. It is crucial to develop robust safeguards and ethical guidelines to ensure that AI systems are used responsibly and that patient safety remains the top priority. As Dr.Eric Topol of Scripps Research noted in 2020, “AI is coming to medicine, but it’s not going to replace doctors. It’s going to augment them.” This perspective underscores the importance of viewing AI as a tool to enhance human capabilities rather than a replacement for human expertise.
In the United States, healthcare providers are increasingly exploring the use of AI-powered tools for various applications. For instance, AI algorithms are being used to analyze radiology images to detect tumors and other abnormalities, to predict patient outcomes based on their medical history, and to personalize treatment plans based on individual patient characteristics. Though, the adoption of AI in healthcare is still in its early stages, and there is a need for further research to validate its effectiveness and ensure its safe and equitable deployment.
Navigating the Hype: A Call for Critical evaluation
The enthusiasm surrounding AI in medicine can sometimes overshadow the practical challenges and limitations. Experts caution against blindly accepting AI solutions without rigorous evaluation and validation.It is indeed essential to critically assess the accuracy, reliability, and generalizability of AI algorithms before deploying them in clinical settings.
One of the key challenges is the “black box” nature of some AI algorithms,particularly deep learning models. These models can be highly complex and difficult to interpret, making it challenging to understand how they arrive at their conclusions. This lack of transparency can raise concerns about accountability and trust, especially in high-stakes medical decisions.
Another concern is the potential for algorithmic bias. AI algorithms are trained on data, and if that data reflects existing biases in healthcare, the algorithms may perpetuate or even amplify those biases. For example, if an AI algorithm is trained primarily on data from one demographic group, it may not perform as well on patients from other demographic groups.
To address these challenges, it is crucial to develop methods for evaluating and validating AI algorithms in a rigorous and transparent manner. This includes testing the algorithms on diverse patient populations, assessing their performance against established benchmarks, and developing techniques for explaining their decision-making processes. As the National Institutes of Health (NIH) has emphasized, “AI has the potential to transform healthcare, but only if it is developed and used responsibly.”
In the U.S. context,this means ensuring that AI systems comply with regulations such as HIPAA (Health Insurance Portability and Accountability Act) and that they are designed to promote health equity. Healthcare providers also need to invest in training and education to ensure that their staff are equipped to use AI tools effectively and to interpret their results accurately.
Real-World applications and Future Directions
Despite the challenges, AI is already demonstrating its potential to improve healthcare in various ways. Here are some real-world examples of AI applications in medicine:
- Diagnostics: AI algorithms can analyze medical images, such as X-rays and MRIs, to detect diseases like cancer and Alzheimer’s with high accuracy.
- Drug Discovery: AI can accelerate the drug discovery process by identifying potential drug targets and predicting the efficacy of new drug compounds.
- Personalized Medicine: AI can analyze patient data to tailor treatment plans to individual patient characteristics, improving outcomes and reducing side effects.
- Remote Patient Monitoring: AI-powered wearable devices can monitor patients’ vital signs and alert healthcare providers to potential problems,enabling timely intervention.
- Administrative Tasks: AI can automate administrative tasks,such as scheduling appointments and processing insurance claims,freeing up healthcare professionals to focus on patient care.
Looking ahead, the future of AI in medicine is bright. As AI technology continues to advance and as more data becomes available, we can expect to see even more innovative applications of AI in healthcare. However, it is essential to proceed with caution, ensuring that AI is used responsibly and ethically and that patient safety remains the top priority.
One promising area of research is the development of “explainable AI” (XAI) techniques. XAI aims to make AI algorithms more transparent and interpretable, allowing clinicians to understand how they arrive at their conclusions. this can definitely help to build trust in AI systems and to identify potential errors or biases.
Another important area of focus is the development of AI ethics guidelines and regulations. These guidelines should address issues such as data privacy, algorithmic bias, and accountability. They should also ensure that AI systems are used in a way that promotes health equity and that does not discriminate against any particular group of patients.
Expert Perspectives
Several leading experts in the field have weighed in on the promises and perils of AI in medicine. Here are some notable quotes:
AI is coming to medicine, but it’s not going to replace doctors. It’s going to augment them.Dr.Eric Topol, Scripps Research
AI has the potential to transform healthcare, but only if it is developed and used responsibly.National Institutes of Health (NIH)
Data table: AI in Healthcare – Potential Benefits and Challenges
| Area | Potential Benefits | Challenges |
|---|---|---|
| Diagnostics | Improved accuracy, faster detection | Data bias, “black box” algorithms |
| Drug Discovery | Accelerated development, targeted therapies | Validation, regulatory hurdles |
| Patient Care | Personalized treatment, remote monitoring | Privacy concerns, data security |
| Administration | Automation, reduced costs | job displacement, implementation costs |
AI’s Expanding Role in Healthcare: From Diagnosis to Personalized Treatment
Recent advancements in artificial intelligence are revolutionizing healthcare,offering new tools for diagnosis,treatment,and patient care. But are we ready?
The AI Revolution in Medicine: A Closer Look
Artificial intelligence is no longer a futuristic fantasy; it’s rapidly transforming the landscape of healthcare in the United states. From assisting doctors in making more accurate diagnoses to personalizing treatment plans and streamlining administrative tasks, AI’s potential is vast. But with such rapid advancements come critical questions about data privacy, algorithmic bias, and the future role of human clinicians.
One of the most promising applications of AI lies in its ability to analyze complex medical data with unparalleled speed and precision. Imagine a scenario where a patient presents with a constellation of symptoms that might point to several different conditions. Traditionally, a doctor would need to order a series of tests, each taking time and resources, to narrow down the possibilities. Though, an AI-powered diagnostic tool could sift through the patient’s medical history, lab results, and even genomic information to quickly identify the most likely diagnosis.
This isn’t just theoretical. Several companies are already developing AI-powered diagnostic tools for a range of conditions, from cancer to heart disease. Such as, IBM’s Watson Oncology has been used in some hospitals to assist oncologists in developing treatment plans for cancer patients. While these tools are not meant to replace human doctors, they can provide valuable insights and help clinicians make more informed decisions.
Beyond Diagnosis: AI in treatment and Patient Care
AI’s impact extends far beyond diagnosis. It’s also being used to develop personalized treatment plans tailored to individual patients. By analyzing a patient’s unique genetic makeup, lifestyle, and medical history, AI can help doctors predict how they will respond to different treatments and identify the most effective course of action.
Consider the case of a patient with diabetes. An AI-powered system could monitor their blood glucose levels, diet, and activity levels in real-time, providing personalized recommendations for managing their condition. This could include suggesting specific foods to eat, recommending optimal exercise routines, or even adjusting insulin dosages as needed.
Furthermore, AI is being used to improve patient care in a variety of ways, such as:
- Remote patient monitoring: AI-powered devices can track patients’ vital signs and alert doctors to potential problems before they become serious.
- Virtual assistants: Chatbots can answer patients’ questions, schedule appointments, and provide medication reminders.
- Drug discovery: AI can accelerate the process of identifying and developing new drugs by analyzing vast amounts of data and predicting which compounds are most likely to be effective.
Addressing the challenges: ethical Considerations and the Future of AI in Healthcare
While the potential benefits of AI in healthcare are undeniable, there are also significant challenges that need to be addressed. One of the biggest concerns is data privacy. As AI systems become more sophisticated, they require access to vast amounts of patient data. It’s crucial to ensure that this data is protected from unauthorized access and misuse.
Another concern is algorithmic bias. AI algorithms are trained on data, and if that data reflects existing biases, the algorithms will perpetuate those biases. This could lead to disparities in healthcare outcomes, with certain groups of patients receiving less effective treatment.
Such as, if an AI-powered diagnostic tool is trained primarily on data from white patients, it might potentially be less accurate when diagnosing conditions in patients from other racial or ethnic groups. It’s important to ensure that AI systems are trained on diverse datasets and that algorithms are carefully audited to identify and mitigate potential biases.
The rise of AI in healthcare also raises questions about the future role of human clinicians. Will AI eventually replace doctors and nurses? Most experts believe that AI will not replace human clinicians entirely, but rather augment their capabilities.
Dr. Emily Carter, a leading expert in medical AI at the University of California, San Francisco, argues that, “AI can free up doctors and nurses to focus on the most critically important aspects of patient care, such as building relationships, providing emotional support, and making complex ethical decisions.”
Ultimately,the accomplished integration of AI into healthcare will require a collaborative effort between clinicians,data scientists,policymakers,and patients. We need to develop clear ethical guidelines, ensure data privacy and security, and address algorithmic bias to maximize the benefits of AI while minimizing the risks.
Real-World Examples and Case Studies
To illustrate the practical applications of AI in healthcare,here are a few real-world examples:
| Application | Description | Impact |
|---|---|---|
| AI-powered Diagnostics | Systems like IBM Watson Oncology assist doctors in diagnosing cancer and developing treatment plans. | Improved accuracy, faster diagnosis, and personalized treatment recommendations. |
| Remote Patient Monitoring | wearable devices and sensors track patients’ vital signs and alert doctors to potential problems. | Early detection of health issues, reduced hospital readmissions, and improved patient outcomes. |
| Virtual Assistants | Chatbots answer patients’ questions, schedule appointments, and provide medication reminders. | Increased patient engagement, improved access to care, and reduced administrative burden. |
| Drug Discovery | AI algorithms analyze vast amounts of data to identify promising drug candidates. | Accelerated drug development, reduced costs, and more effective treatments. |
Recent Developments and Future Trends
The field of AI in healthcare is constantly evolving. Some of the most recent developments include:
- Advancements in Natural Language Processing (NLP): NLP is enabling AI systems to better understand and interpret medical text, such as electronic health records and research papers.
- Increased use of machine learning: Machine learning algorithms are becoming more sophisticated, allowing AI systems to learn from data and improve their performance over time.
- growing adoption of cloud computing: Cloud computing is providing the infrastructure needed to store and process the vast amounts of data required for AI-powered healthcare applications.
Conclusion: Embracing the Future of Healthcare
AI has the potential to transform healthcare in profound ways, but it’s important to approach this technology with caution and a clear understanding of its limitations. By addressing the ethical challenges, ensuring data privacy and security, and promoting collaboration between humans and machines, we can harness the power of AI to improve the health and well-being of all Americans.
AI’s Expanding Role in Biomedical Research: Revolutionizing Text Analysis and Data Extraction
Published: October 26, 2024
By Archyde News Staff
artificial intelligence (AI) is rapidly transforming biomedical research, particularly in how researchers analyze vast amounts of text and extract crucial data. this article delves into the advancements, challenges, and potential future applications of AI in this critical field, with a focus on its implications for U.S. healthcare and research institutions.
the Rise of AI in biomedical Text Mining
The sheer volume of biomedical literature – research papers, clinical trial reports, and patient records – is overwhelming for human researchers. AI-powered tools are emerging as indispensable allies, capable of sifting through this data deluge to identify patterns, relationships, and insights that would otherwise remain hidden. This capability is particularly relevant in the U.S., where the National Institutes of Health (NIH) alone funds thousands of research projects annually, generating a massive influx of new data.
One key area is biomedical text simplification. Researchers like those at the University of Pittsburgh are working on AI models to make complex medical information more accessible. This is especially important for patient education and ensuring informed consent. Imagine a future where every patient can easily understand the details of their treatment plan,thanks to AI-powered summaries and explanations.
Relation extraction, which identifies relationships between entities like genes, drugs, and diseases, is another crucial application. Companies like IBM Watson health are leveraging AI to accelerate drug discovery by uncovering hidden connections in scientific literature. This could lead to faster development of new treatments for diseases like cancer and Alzheimer’s.
Key Applications and Recent Developments
1. Enhanced Literature Review and Summarization
AI algorithms can automatically generate summaries of research papers, saving researchers considerable time and effort. These tools can also identify relevant articles based on specific keywords or research questions. For example, a researcher studying the effects of a new drug on diabetes could use AI to quickly find and summarize all relevant studies published in the last year.
Recent advancements include the development of models that can summarize long documents more accurately and factually. The LongDocFACTScore
developed in 2024, represents a significant step forward in ensuring the reliability of AI-generated summaries.
2. Improved Data Extraction and Knowledge Graph Construction
AI can extract structured data from unstructured text, such as protein-protein interactions or drug-target relationships. This information can then be used to build knowledge graphs, which are visual representations of complex biological systems. These graphs can help researchers identify potential drug targets or understand the mechanisms of disease.
Companies like Google are investing heavily in knowledge graph technology, recognizing its potential to revolutionize healthcare and other industries. Their Knowledge Graph, for instance, provides information about diseases, symptoms, and treatments directly in search results, improving access to reliable health information for the general public.
3. accelerating Drug Discovery and Development
By analyzing vast amounts of data, AI can identify potential drug candidates and predict their efficacy and safety. This can significantly speed up the drug discovery process, which typically takes many years and costs billions of dollars. Several pharmaceutical companies are already using AI to identify new targets for cancer therapy and to repurpose existing drugs for new indications.
Insitro,a U.S.-based company founded by Daphne Koller, is a prime example of how AI is being used to transform drug discovery. They use machine learning to analyze patient data and identify subpopulations that are more likely to respond to specific treatments.
Challenges and Considerations
Despite the immense potential of AI in biomedical research,several challenges remain. One major concern is the accuracy and reliability of AI models. if the data used to train these models is biased or incomplete, the results may be misleading or even harmful. Ensuring the fairness and transparency of AI algorithms is crucial, especially in healthcare applications.
Another challenge is the lack of standardization in data formats and terminologies. This makes it difficult to integrate data from different sources and to compare the results of different studies. Efforts are underway to develop common data standards and ontologies,but more work is needed in this area.
Ethical considerations are also paramount. As AI becomes more integrated into healthcare, it is indeed essential to address issues such as data privacy, algorithmic bias, and the potential for job displacement. The U.S. government is actively working on developing ethical guidelines and regulations for the use of AI in healthcare.
Expert Perspectives
Leading researchers in the field emphasize the importance of collaboration between AI experts and biomedical scientists. “The key to unlocking the full potential of AI in biomedical research is to bring together experts from different disciplines,” says Dr.Emily Carter, Director of Biomedical Informatics at UCLA. “We need to combine the power of AI with the deep biological knowledge of human experts to make truly transformative discoveries.”
Dr. David Jones, a professor of computer science at Stanford University, adds, “AI is not meant to replace human researchers, but to augment their abilities. By automating tedious tasks and uncovering hidden patterns, AI can free up researchers to focus on the more creative and strategic aspects of their work.”
Future Directions and Implications for the U.S.
the future of AI in biomedical research is bright, with many exciting possibilities on the horizon. As AI models become more sophisticated and data becomes more abundant, we can expect to see even more breakthroughs in areas such as drug discovery, personalized medicine, and disease prevention. This has significant implications for the U.S., which is a global leader in biomedical research and healthcare innovation.
The widespread adoption of AI in healthcare could lead to lower healthcare costs, improved patient outcomes, and a more efficient healthcare system. Though, realizing this potential will require addressing the challenges and ethical considerations outlined above.It will also require investing in education and training to ensure that healthcare professionals have the skills they need to work with AI-powered tools.
Furthermore, the U.S. needs to foster a regulatory environment that encourages innovation while protecting patient safety and privacy. The FDA is actively exploring how to regulate AI-based medical devices and algorithms, and it is indeed likely that new regulations will be introduced in the coming years.
Real-World Examples and Case Studies
Here are some examples highlighting the practical applications of AI in biomedical research within the U.S.:
| Application Area | Example | Impact |
|---|---|---|
| Drug Discovery | Atomwise uses AI to screen virtual libraries of molecules for potential drug candidates. | Accelerated identification of potential treatments for Ebola and multiple sclerosis. |
| Personalized Medicine | Tempus analyzes genomic and clinical data to personalize cancer treatment. | Improved treatment selection and patient outcomes for cancer patients. |
| Disease Diagnosis | IDx-DR uses AI to diagnose diabetic retinopathy from retinal images. | Increased access to screening for diabetic retinopathy, preventing vision loss. |
| Clinical Trial Optimization | Deep 6 AI uses AI to identify eligible patients for clinical trials. | Reduced enrollment times and costs for clinical trials. |
Decoding Google’s E-E-A-T: A Guide for Creating Helpful Content
By Archyde News on April 6, 2025
Understanding E-E-A-T: More Than Just a Ranking Factor
In the ever-evolving landscape of search engine optimization (SEO), understanding Google’s ranking criteria is paramount. While algorithms constantly change, one concept has remained consistently critically important: E-E-A-T. This acronym, standing for Experience, Expertise, Authoritativeness, and Trustworthiness, isn’t a direct ranking factor but rather a set of guidelines used by Google’s quality raters to evaluate the overall quality of web pages.
The Core of E-E-A-T: Being Helpful
While E-E-A-T might seem complex, the underlying principle is simple: be helpful. Content that genuinely addresses user needs and provides valuable information is more likely to perform well in search results.This means understanding your audience, anticipating their questions, and providing clear, accurate, and insightful answers.
According to recent news, Google’s E-E-A-T guidelines are indeed a “set of criteria for the people at Google who verify content quality.”
Think of it this way: if you were asking a friend for advice, you’d want someone with relevant experience, deep knowledge, a respected reputation, and, above all, someone you trust. Google applies a similar logic to its search results.
Consider a website offering financial advice. To meet E-E-A-T standards, the site should demonstrate:
- Experience: The authors should have practical experience in finance, such as managing investments or working as financial advisors.
- Expertise: They should possess in-depth knowledge of financial concepts and strategies, demonstrated through certifications, publications, or detailed explanations.
- Authoritativeness: The site should be recognized as a reliable source of financial information by other reputable organizations or experts.
- Trustworthiness: The site should be transparent about its sources of information, disclose any potential conflicts of interest, and have a clear privacy policy.
E-E-A-T as a Guide for Content Creation
E-E-A-T isn’t just for Google’s quality raters; it’s also a valuable framework for content creators. By focusing on these principles, marketers can create content that is more likely to rank higher in search engine results pages (SERPs). As the original article noted, “it’s also a great guide for marketers to help them create content that has a better chance of landing high up on SERPs.”
Here are some practical tips for incorporating E-E-A-T into your content strategy:
- Know Your Audience: Understand their needs, pain points, and search queries. Conduct thorough keyword research to identify the topics they’re interested in.
- Create High-Quality Content: Focus on providing accurate, informative, and engaging content that addresses user needs. Avoid thin content, keyword stuffing, and other black-hat SEO tactics.
- Cite Your Sources: Back up your claims with credible sources, such as peer-reviewed studies, government reports, and reputable news organizations.
- Build Your Reputation: Earn backlinks from other authoritative websites in your industry. Participate in industry events and engage with your audience on social media.
- Be Transparent: Clearly identify the authors of your content, and disclose any potential conflicts of interest. Make it easy for users to contact you with questions or concerns.
- Prioritize User Experience: Ensure your website is easy to navigate, mobile-pleasant, and loads quickly. A positive user experience is crucial for building trust and credibility.
Recent Developments and Additional Insights
Google continually refines how it assesses E-E-A-T. Recent updates emphasize the importance of “real-world” experience, particularly for topics that directly impact people’s lives, such as health, finance, and safety. This is especially crucial in the age of AI-generated content. Google is increasingly looking for signals that content was created by someone with genuine expertise and experience in the subject matter.
Furthermore, the rise of misinformation and “fake news” has made trustworthiness an even more critical factor. Websites need to demonstrate a commitment to accuracy, transparency, and ethical practices to earn the trust of both Google and their audience.
Consider the impact on the healthcare industry. A blog post claiming a miracle cure without scientific basis would violate the principles of E-E-A-T, potentially harming readers who rely on the information. legitimate healthcare providers and organizations must prioritize evidence-based content and transparency to maintain credibility.
| E-E-A-T Factor | Key Considerations | U.S. Example |
|---|---|---|
| Experience | Practical knowledge and life experiences. | A chef writing a cookbook with recipes perfected over years in a restaurant. |
| Expertise | In-depth knowledge and skills in a specific area. | A certified financial planner providing investment advice. |
| Authoritativeness | Recognition as a reliable source of information. | The Mayo Clinic website for health information. |
| Trustworthiness | honesty,transparency,and ethical practices. | A news organization with a clear corrections policy. |
Addressing Potential Counterarguments
Some critics argue that E-E-A-T is subjective and difficult to measure. While it’s true that assessing qualities like “trustworthiness” can be challenging, Google’s quality raters use a comprehensive set of guidelines and signals to evaluate websites. Furthermore, E-E-A-T aligns with fundamental principles of good journalism and ethical content creation.
Another counterargument is that focusing on E-E-A-T can stifle creativity and originality. However, this is a misconception. E-E-A-T doesn’t require content to be bland or formulaic. instead, it encourages creators to produce engaging and informative content that is also accurate and trustworthy.
As an archyde.com journalist, I strive to find additional insights by looking at trends in other related content.
Practical applications and the Future of E-E-A-T
E-E-A-T is not a passing fad but a fundamental aspect of Google’s approach to search. As algorithms become more sophisticated, the ability to create high-quality, trustworthy content will become even more critical. Businesses and organizations that prioritize E-E-A-T will be well-positioned to succeed in the long term.
For U.S. businesses, this means focusing on building a strong online reputation, investing in quality content creation, and prioritizing user experience. By embracing E-E-A-T, companies can not only improve their search engine rankings but also build trust with their customers and establish themselves as leaders in their respective industries.