2024-04-26 21:42:10
welcome to Impact factor, your weekly dose of commentary on a new study in medicine. I am Dr. F. Perry Wilson, from the Yale School of Medicine, in New Haven, USA.
Today it’s a battle of the sexes as we dive into an article that makes you say, “Wow, that’s an interesting study” and also “wow, I’m glad I didn’t do that study.” And studies of this kind are always somewhat delicate; They say something regarding medicine, but also regarding society and that makes this a bit delicate. But that has never stopped us. So let’s try to answer the question: are female doctors better than male doctors?
On the surface, this question is almost impossible to answer. It is too broad: what does it mean to be a “better” doctor? At first glance, it appears that there are too many variables to control: type of doctor, type of patient, clinical scenario, etc.
But in this study what compared mortality and hospital readmission rates by doctor and patient’s gender, published in Annals of Internal Medicine, A rather ingenious method is used to eliminate all bias by taking advantage of two simple facts:[1] First, hospital medicine today is largely in the hands of hospitalists; Second, because their work is based on shifts, it is practically random which hospitalist you get when you enter a hospital.
In other words, if you are admitted for an acute illness and are seen by a hospital doctor, you have no control over whether they are male or female. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults age 65 and older who had nonelective hospitalizations in the United States. The claims revealed the gender of the patient and the name of the doctor who treated him. Through a link to a database of medical providers, they were able to determine the gender of the attending physician.
The aim was to analyze the results of four dyads:
-
Male patient-male doctor.
-
Male patient-female doctor.
-
Female patient-male doctor.
-
Female patient-female doctor.
The primary endpoint was 30-day mortality.
I’ve already told you that focusing on hospitalists introduces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by 50,000 doctors, 30% of whom were women. And while female and male patients were different, the same was not true of the gender of their hospitalist. Based on physician gender, patients were therefore similar in mean age, race, ethnicity, family income, Medicaid eligibility, and comorbidities. The authors even created a “predicted mortality” score that was also similar across groups.
Now, female doctors were a little different than male doctors. Female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year and were slightly younger.
So we have very similar patients, regardless of who their hospitalist was, but hospitalists are different due to factors other than gender. Good.
Here I have drawn the results. The 30-day mortality rate for female patients was significantly lower than for male patients, but they fared even better when seen by female doctors than by male doctors. The doctor’s gender did not affect the results of the male patients to a large extent. The secondary endpoint (30-day hospital readmission) showed a similar trend.
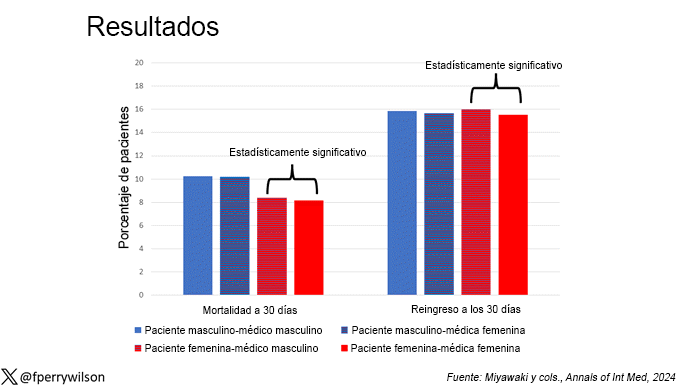
This is a relatively small effect, no doubt, but if we multiply it by millions of annual hospital admissions, we can start to get real numbers.
So what’s going on here? I see four broad groups of possibilities.
Let’s start with the obvious explanation: women are, on average, better doctors than men. I am married to a doctor and from my personal experience this explanation is undoubtedly true. But why?
The authors cite data indicating that female doctors are less likely than male doctors to disregard patients’ concerns – especially female patients – which may lead to fewer missed diagnoses.[2] But this is impossible to measure with administrative data, so this study cannot tell us whether female hospitalists are more attentive than their male counterparts, nor can it indicate that the advantage is mediated by the shorter average height of female doctors. Perhaps the key is to be closer to the patient?
The other possibility here is that this has nothing to do with the doctor’s gender at all; It has to do with other things related to the doctor’s gender. We know, for example, that female doctors saw fewer patients per year than male doctors, but the study authors took this into account in the statistical models. Nevertheless, there may be other unmeasured factors (confounding factors). By the way, confounding factors will not necessarily change the main conclusion: es Better that women serve you. It is not Because they are women, it is a convenient marker for another quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea in this case is that doctors only enter the study if they are hospital doctors and the quality of the doctors who choose to be hospital doctors can vary depending on gender. When deciding on a specialty, a talented resident who considers certain aspects of their lifestyle may find hospital medicine particularly attractive, and that the attraction toward a more lifestyle-friendly specialty may differ by gender, as some previous studies have shown.[3] If true, the group of female hospitalists may be better than their male counterparts, because doctors of that caliber do not become hospitalists.
Well, don’t take that into account. I’m just trying to give examples of how to think regarding collider bias. I can’t prove this is the case, and in fact the authors do a sensitivity analysis of all doctors, not just hospitalists and show the same thing. So it’s probably not true, but epidemiology is fun, right?
And the fourth possibility: this is nothing but statistical noise. The effect size is incredibly small and right on the edge of statistical significance. Especially when working with very large data sets like this, one must be very careful not to overinterpret statistically significant findings that are nevertheless of small size.
Regardless, it’s an interesting study that made me reflect and, of course, worry a little regarding how to present it. Forgive me if I have been insensitive in addressing the complex issues of sex, gender and society here. After all, I’m just a male doctor.
El Dr. F. Perry Wilson, MSCE, (@fperrywilson) is an associate professor of medicine and director of the Yale Clinical and Translational Research Accelerator. Her science communication work can be found on the Huffington Post, on NPR, and here on Medscape. Your new book, How medicine works and when it doesn’t work, It is now available.
This content was originally published in the English edition of Medscape.
1714180806
#female #doctors #male #doctors