© Provided by LA Times
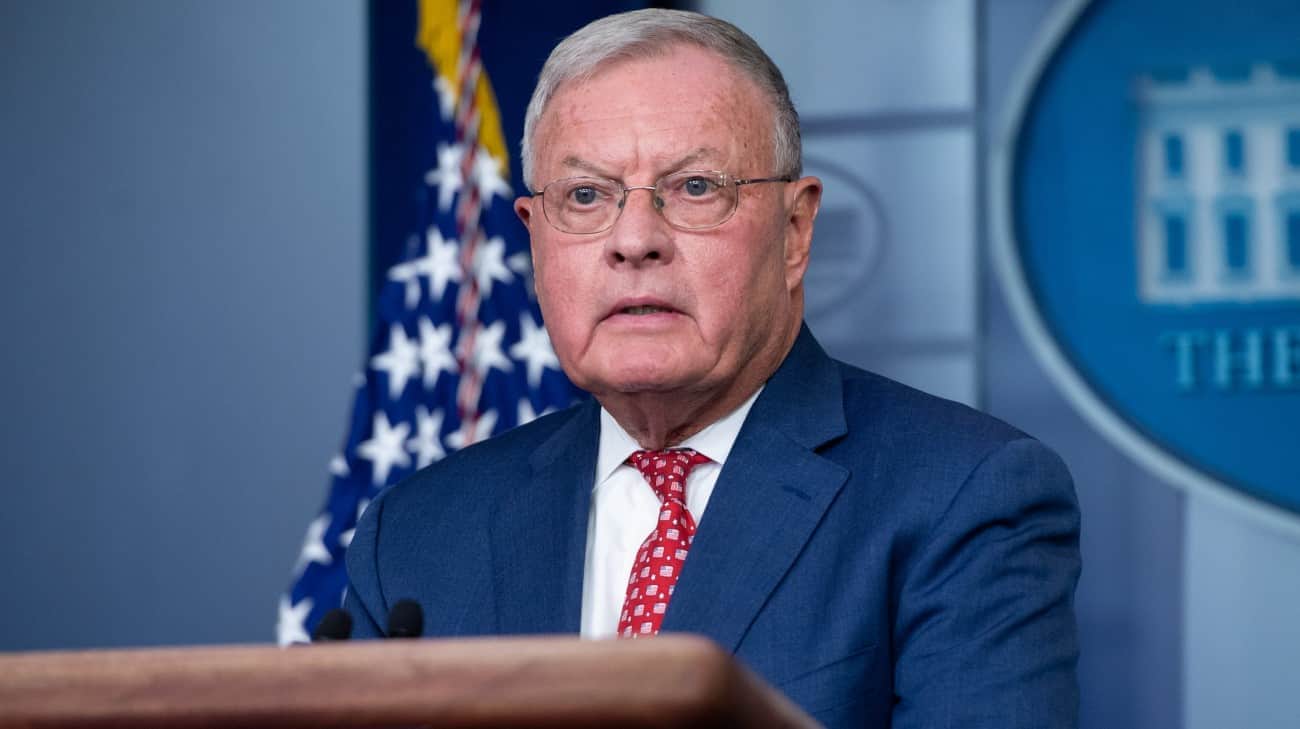
Dr. Troy Pennington attends to a patient brought to the emergency room at Arrowhead Regional Medical Center on January 11. The recent increase in COVID-19 cases and a shortage of healthcare personnel have put the care of those hospitalized at the Colton center to the test. (Irfan Khan/Los Angeles Times)
Even as Omicron’s winter surge reaches its climax, Los Angeles County health officials are urging residents to continue to avoid nonessential gatherings, saying coronavirus transmission remains at one of the highest levels never seen in the history of the 2-year pandemic.
Despite recent declines, California is seeing an average of more than 100,000 new coronavirus cases a day, more than double last winter’s peak of 46,000. The latest figure represents an extraordinary level of transmission that shows that there are many more people infected and infected simultaneously than at any previous point in the pandemic.
So while officials express hope that California’s winter surge is finally cresting and, in some areas, beginning to recede, Los Angeles County Public Health Director Barbara Ferrer said it remains being prudent to postpone non-essential activities in which people are without masks and in close contact with each other, such as dinners and parties.
“We have to be extraordinarily cautious when there’s so much community transmission. We’ve actually never had this many infections at any other time in the pandemic,” Ferrer explained. “It is extraordinarily easy to be exposed. Although many of those people who have been infected will not have major problems, others are in our hospitals fighting for their lives.”
Los Angeles County reported 102 new COVID-19 deaths Thursday, the highest single-day total since March 10, 2021. Weekly rates of deaths from the coronavirus have doubled in recent weeks in both the jurisdiction as well as the state as a whole, although they are still less than a quarter of those seen during the worst of last winter, likely due to levels of immunity generated by vaccinations and previous viral exposure.
Hospitalizations have also increased dramatically during the Omicron wave. The total number of people with coronavirus who required hospitalization in California increased 15% in the last week, reaching 15,383 on Thursday. Of those patients, 2,485 are in intensive care units, a figure that has increased 21% in the last seven days.
However, the number of hospitalizations of this type throughout the state decreased slightly from Wednesday to Thursday, with a decrease of 10 patients.
This decline, albeit slight, comes following a spike of regarding a month in which the number of hospitalized coronavirus patients in California more than quadrupled.
Some of the state’s most populous counties, including Los Angeles, San Diego, San Bernardino, Orange and Riverside, also saw slight daily declines in patient numbers.
While unvaccinated people are at greatest risk of being hospitalized due to COVID-19, inoculated residents with underlying health conditions can still become infected and suffer serious illness, especially if they don’t have a booster dose.
“Between the increase in deaths and hospitalizations, there should be no room for complacency,” Ferrer said. “Although Omicron is not causing the same proportion of serious illness as last winter… it is growing. And for a growing number of people in Los Angeles County, that variant of COVID-19 has now become a critical issue of life or death”.
The death rate from COVID-19 in the last month has varied in different parts of the state.
As of Thursday, San Francisco had reported 20 COVID-19 deaths since New Year’s Day, meaning that for every 100,000 residents, 2.3 people have died, according to state data. In contrast, Los Angeles County reported at least 667 deaths in the same period, which means that, for every 100,000 inhabitants, 6.6 have died.
San Francisco’s chief health officer, Dr. Grant Colfax, blamed the city’s high rate of booster dosing as a key reason behind its low COVID-19 death rate in January. About half of San Francisco residents have received a booster shot. In Los Angeles County, just under a third of Angelenos have been vaccinated.
“Fortunately, in the vast majority of our infections in the city, the cases have been mild – because people were fully vaccinated with the first series, and many people were up to date on their doses regarding boosters,” Colfax said.
The official still urged residents to be vigilant, noting that hospitalizations continue to rise.
But unlike Southern California, where overcrowded emergency rooms struggle to maintain care and some patients wait days for a hospital bed, San Francisco’s hospitals appear to have the capacity to handle the demand.
Colfax cited San Francisco’s much lower death rate as one reason he’s ready to talk regarding a post-winter surge future, in which the public health department’s goal “is not to prevent every case of COVID “, but rather “notice the worst outcomes, serious illnesses, hospitalizations and death”.
As cases decline, Colfax said, San Francisco plans to make decisions to remove certain pandemic restrictions “when and where it makes sense.”
“And while it is certainly possible and plausible that we will face other variants in the future, hopefully we will be able to place COVID among the many other infectious diseases and health conditions that we have to deal with, intelligently, not letting it disrupt our lives,” he explained.
Hospitals in Southern California, meanwhile, appear to be doing relatively worse than those in the Bay Area.
Many downstate health care systems have been forced to postpone some scheduled surgeries or procedures to cope with a surge in hospital demand and a shortage of health care workers. Ambulance response times to 911 calls have worsened as the surge intensified.
“The health care system is really overwhelmed,” said Dr. Clayton Chau, director of the Orange Health Care Agency. “We are praying that our ICU capacity is not overwhelmed.”
Ferrer suggested that it was not yet time to stop worrying regarding new coronavirus infections, given that Los Angeles County hospitals remain “under enormous pressure.”
Advances that would help the region include a plentiful supply of COVID drugs, which have just become available but remain severely limited for now, and addressing problems with access to coronavirus testing.
It is important to maintain caution and make efforts to avoid contagion, Ferrer said.
“I have also heard from many people, who say: ‘Oh, Ómicron is not serious. There is no need to worry. I am not going to take many precautions. Everyone is going to have Ómicron. And let’s get it over with,'” Ferrer said. . “I am firmly of the position that that is an inappropriate response for where we are in the pandemic.”
There are plenty of reasons to remain concerned regarding infection, he noted. There is the possibility of prolonged COVID, in which symptoms can persist for months, if not longer; just as it is possible that child survivors of COVID-19 will later become ill with multisystem inflammatory syndrome, a rare but serious complication that can cause death.
“So I think people should get vaccinated once morest COVID. I think when it comes to a vaccine-preventable disease, not doing it is the wrong strategy,” Ferrer said.
He added that vaccines appear to provide a better level of protection once morest reinfection than surviving COVID-19 without inoculation.
“People who got infected with Delta, it turns out, have high rates of re-infection with Omicron,” Ferrer said.
And even the illness caused by COVID-19, even if it does not require hospitalization, can result in miserable suffering.
“You can talk to people who are awake three or four nights in a row: Yes, they’re at home, they’re not in the hospital. But they can’t sleep because they’re coughing, or they’ve lost their sense of taste and smell for weeks,” Ferrer says. . “Either they’ve had a fever, or they’re isolating themselves from the people they love for a long period of time, and they’re missing birthday celebrations. So yeah, I think everyone needs to continue to be cautious.”
Ferrer said that taking measures such as avoiding dining in an indoor restaurant or in bars does not have to last a long time, but rather it is regarding overcoming the period of weeks of a surge. “Those are places where the exposure rates can be extraordinarily high, since people are not wearing masks and they are closed,” Ferrer said.
When considering non-essential gatherings, Ferrer said people have to decide if they’re willing to take the risk of infection, or if it’s a better idea to delay the event for a while.
For people thinking of getting together for dinner for the Lunar New Year, which falls on Feb. 1, Ferrer advised being cautious regarding delaying gatherings involving high-risk family members in case they come down with an infection. by coronavirus.
The danger can be reduced by having guests undergo rapid testing before gathering, keeping guests in ventilated and distanced places, and wearing face coverings as much as possible when not eating or drinking.
“But for some people, this is a very risky time,” Ferrer said, especially for older adults, especially those with underlying health conditions or a weakened immune system, or those who remain unvaccinated.
To read this note in English Click here
This article was first published in Los Angeles Times in Spanish.