
Trump’s Plan for US Financial Dominance
HereS a freshly minted,AP-style news feature based on the provided source material,geared for Archyde.com: Trump’s Economic Vision: A MAGA Blueprint for Dollar Dominance and Wall

HereS a freshly minted,AP-style news feature based on the provided source material,geared for Archyde.com: Trump’s Economic Vision: A MAGA Blueprint for Dollar Dominance and Wall
Kyabram, KY, Opens After-Hours, No-Cost GP Clinic to Address Healthcare Gap KYABRAM, Ky. (Archyde.com) — January 3, 2024 Residents of Kyabram, Kentucky, and surrounding Campaspe
US Lagging in Electric Vehicle Adoption Despite Global Growth, Survey Shows by Archyde.com News Service June 7, 2024 While the global adoption of electric vehicles
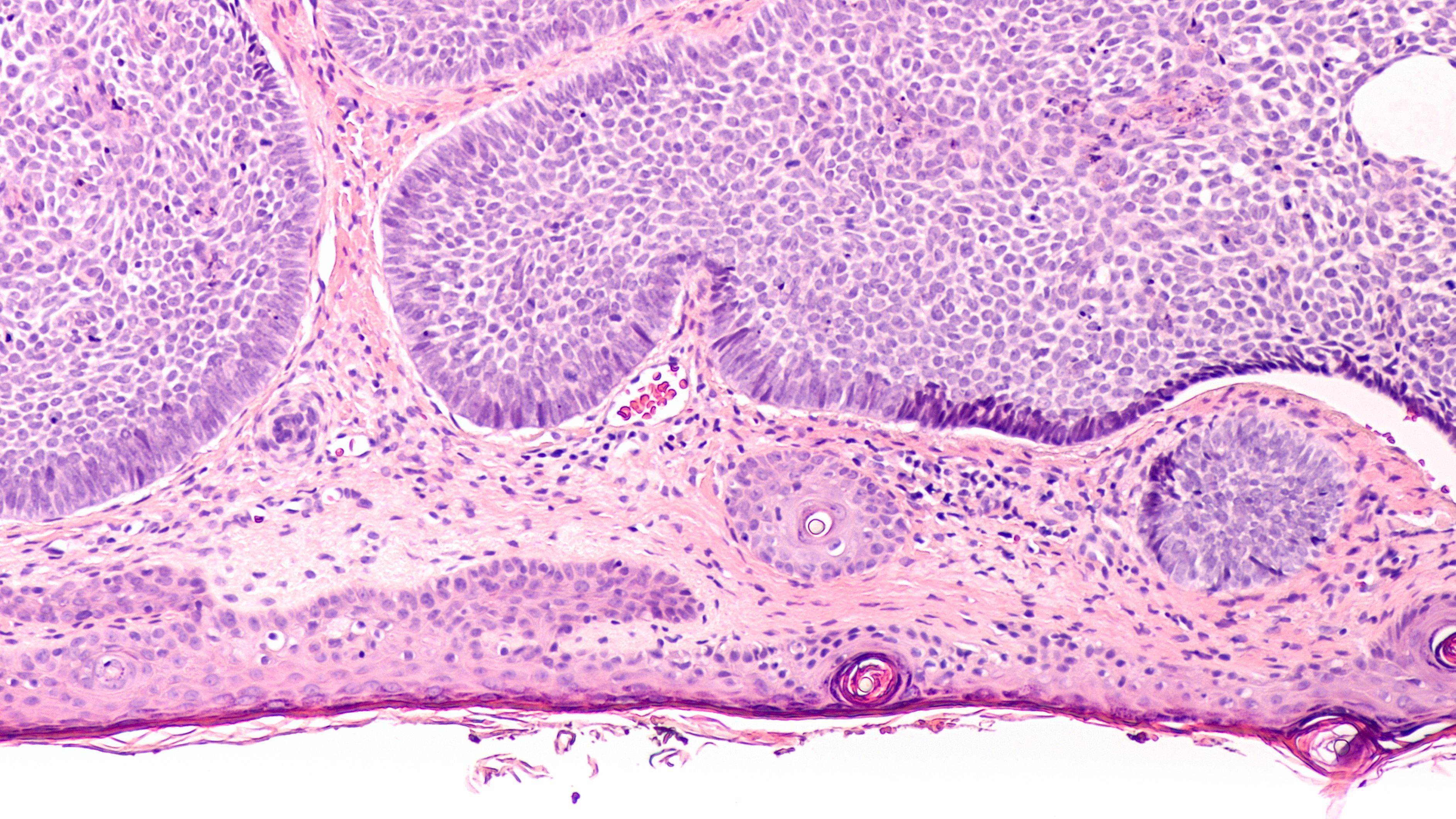
AI Shows Promise in Diagnosing Skin Cancer, Especially Where Pathologists Are Scarce By Archyde News Service April 28, 2025 CHICAGO—Pretrained machine learning models are showing

HereS a freshly minted,AP-style news feature based on the provided source material,geared for Archyde.com: Trump’s Economic Vision: A MAGA Blueprint for Dollar Dominance and Wall
Kyabram, KY, Opens After-Hours, No-Cost GP Clinic to Address Healthcare Gap KYABRAM, Ky. (Archyde.com) — January 3, 2024 Residents of Kyabram, Kentucky, and surrounding Campaspe
US Lagging in Electric Vehicle Adoption Despite Global Growth, Survey Shows by Archyde.com News Service June 7, 2024 While the global adoption of electric vehicles
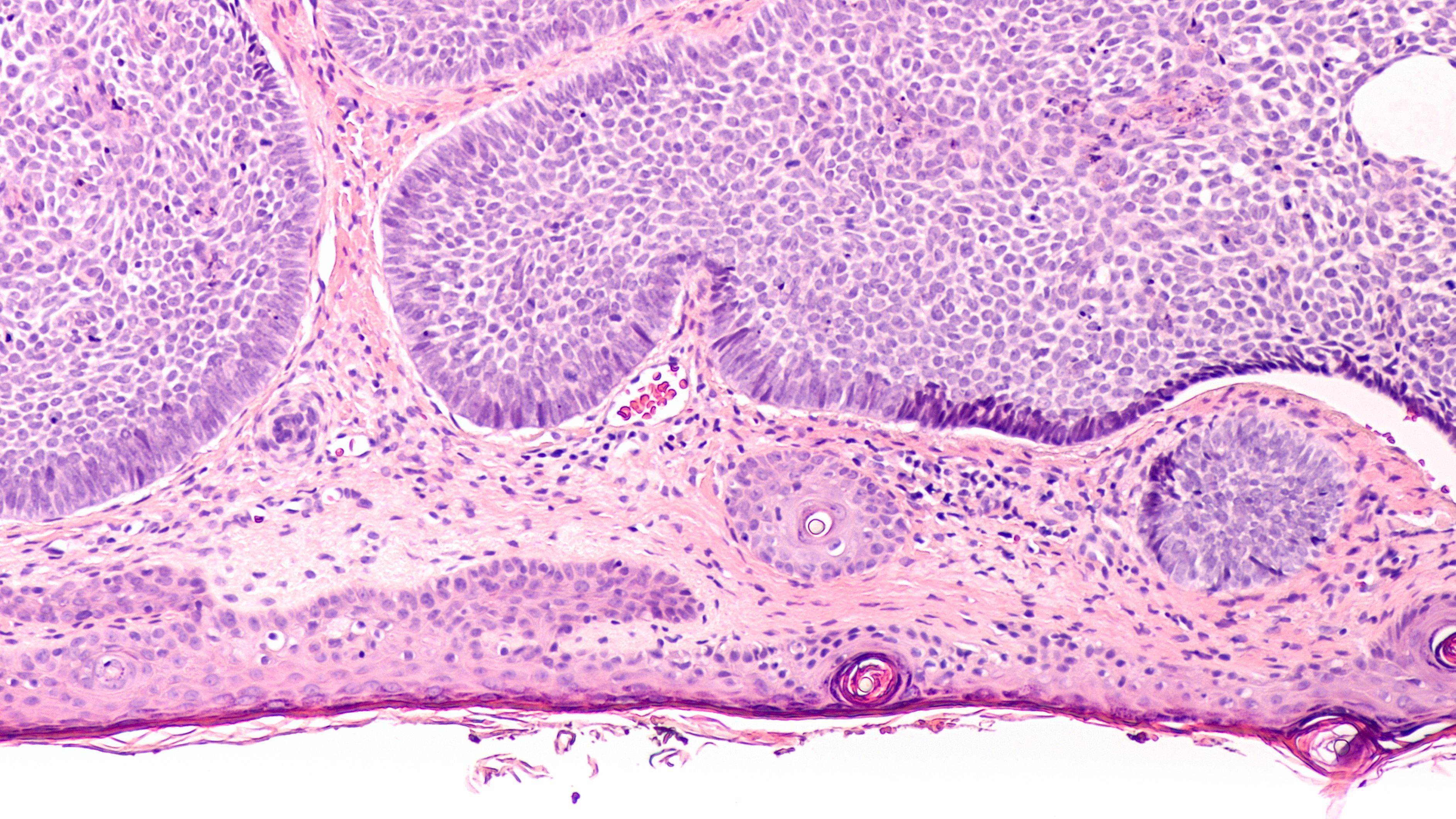
AI Shows Promise in Diagnosing Skin Cancer, Especially Where Pathologists Are Scarce By Archyde News Service April 28, 2025 CHICAGO—Pretrained machine learning models are showing

© 2025 All rights reserved