Streamlining TB Care: A New Tool for Safer, More Efficient Isolation Practices
Table of Contents
- 1. Streamlining TB Care: A New Tool for Safer, More Efficient Isolation Practices
- 2. How might the principles behind “TB or Not TB” be adapted to address other communicable diseases, and what are the potential challenges in doing so?
- 3. Streamlining TB Care: An Interview with Dr. Erica Shenoy
- 4. What inspired the development of the “TB or Not TB” tool?
- 5. How does “TB or Not TB” work, and what sets it apart from existing TB management strategies?
- 6. What are the potential benefits of using “TB or Not TB” for both patients and healthcare professionals?
- 7. What are your thoughts on the potential impact of “TB or Not TB” on the broader healthcare landscape?
- 8. Do you think this tool could be adapted to assess and manage other communicable diseases?
Tuberculosis (TB) cases have been on the rise in recent years, prompting healthcare facilities to implement stringent precautions for patients suspected of having the disease.These precautions frequently enough involve isolating patients in specialized airborne infection isolation rooms, impacting clinical workflows, patient access to care, and hospital capacity. Recognizing this challenge, a team of experts at Massachusetts General Hospital (MGH) developed a novel solution: a clinical decision support tool designed to streamline TB isolation practices, ensuring patient safety while optimizing resource allocation.
“Infection prevention and Control programs play a crucial role in safeguarding patients and healthcare personnel from communicable diseases,” explains dr. Erica Shenoy,Chief of Infection Control at Mass General Brigham and senior author of the study. “However, patient isolation can significantly impact clinical workflows, access to care, and hospital capacity. Therefore, efficient deisolation protocols are essential.”
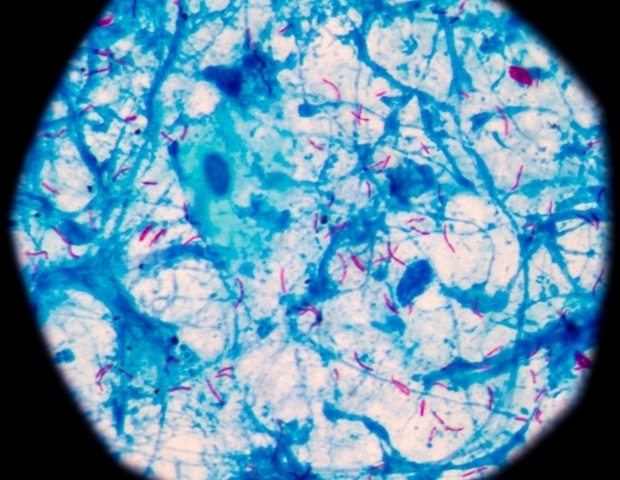
The innovative tool,aptly named “TB or Not TB,” leverages a validated risk scoring model developed by infectious disease physicians and researchers at MGH. This model, trained on extensive patient data, accurately assesses the likelihood of TB infection, guiding clinicians in determining when isolation precautions can be safely discontinued.
When a patient presents with potential TB symptoms, they are flagged as “TB-Risk,” triggering appropriate isolation procedures. Once clinicians, based on patient history, symptoms, and test results, believe TB is unlikely, they can utilize the “TB or Not TB” tool.The tool’s analysis provides clear guidance, allowing clinicians to confidently discontinue isolation precautions for patients deemed low-risk, freeing up valuable resources and improving patient experience.
dr. Caitlin Dugdale,MD,MSc,and Dr. Kimon Zachary, MD, co-lead authors of the study, highlight the tool’s effectiveness: “Our rigorous analysis across six years of TB evaluations at MGB demonstrated that the tool accurately identified all instances of TB infection, ensuring continued safe isolation. Simultaneously,it identified approximately 25% of cases where TB was highly unlikely,enabling safe and efficient deisolation.”
These findings underscore the important impact of “TB or Not TB” on patient care and clinician workflows. By automating the complex decision-making process surrounding TB isolation, the tool reduces cognitive burden, streamlines workflows, and ultimately improves patient outcomes. The tool’s prosperous implementation at all MGB sites serves as a model for othre healthcare institutions seeking to optimize TB management practices.
How might the principles behind “TB or Not TB” be adapted to address other communicable diseases, and what are the potential challenges in doing so?
Streamlining TB Care: An Interview with Dr. Erica Shenoy
Tuberculosis (TB) cases are on the rise, leading to increased anxieties and challenges for healthcare facilities globally. In response to this pressing issue, Dr. Erica Shenoy, Chief of Infection Control at Mass General Brigham, spearheaded a groundbreaking initiative: a clinical decision support tool named “TB or Not TB.” This innovative tool aims to streamline TB isolation procedures, balancing patient safety with optimized resource allocation.Archyde’s health reporter, Archys, spoke with Dr. Shenoy to delve into the complexities of TB management, the impact of this new tool, and its potential implications for the future of healthcare.
What inspired the development of the “TB or Not TB” tool?
“Infection prevention and control programs are vital to safeguarding patients and healthcare staff from infectious diseases like TB,” says Dr. Shenoy. “Though, conventional TB isolation practices can considerably impact clinical workflows, patient access to care, and hospital capacity. We needed a more efficient system to ensure patients receive timely care while minimizing unnecessary isolation periods. The development of ‘TB or Not TB’ was directly born out of this need.”
How does “TB or Not TB” work, and what sets it apart from existing TB management strategies?
“Our tool leverages a validated risk scoring model, meticulously crafted by infectious disease physicians and researchers at MGH. This model, trained on extensive patient data, accurately assesses the likelihood of TB infection based on patient history, symptoms, and test results,” Dr. Shenoy explains. “Clinicians can input the relevant patient data into the tool, and it provides clear, evidence-based guidance on when isolation precautions can be safely discontinued. This removes the ambiguity and potential for human error that often accompany manual decision-making processes.”
What are the potential benefits of using “TB or Not TB” for both patients and healthcare professionals?
“The benefits are multifaceted,” Dr.Shenoy highlights. “For patients, it means shorter isolation periods, reduced disruption to their lives, and improved access to essential healthcare services. For healthcare professionals, it streamlines workflows, reduces cognitive burden, and frees up valuable resources, allowing them to focus on providing quality patient care. Ultimately, the tool empowers clinicians to make confident and informed decisions regarding TB isolation, leading to better patient outcomes and a more efficient healthcare system.”
What are your thoughts on the potential impact of “TB or Not TB” on the broader healthcare landscape?
“We believe ‘TB or Not TB’ represents a important step forward in tackling the challenges posed by TB,” Dr. Shenoy states. ”Our prosperous implementation across all MGB sites serves as a model for other healthcare institutions seeking to optimize TB management practices. Moreover, the tool’s underlying principles—leveraging data and technology to improve clinical decision-making—have wide-ranging applications in addressing other infectious disease challenges.”
Do you think this tool could be adapted to assess and manage other communicable diseases?
“Absolutely,” says Dr. Shenoy. “The core concepts of ‘TB or Not TB’- leveraging data analytics and machine learning to guide clinical decision-making- are highly adaptable to other communicable diseases.We are actively exploring the potential for applying these principles to other infectious threats, and this could revolutionize how we manage and control outbreaks in the years to come.”