The Unsung Heroes of Modern Medicine: A History of Blood Gas Analyzers
Step into any modern hospital, and you’ll be surrounded by the beeping, whirring machinery of advanced medical technology. From X-rays revealing intricate bone structures to fMRI scans painting vibrant portraits of the brain, these marvels of technology capture our imagination. Yet, tucked away amidst the high-tech spectacle are simpler machines, often overlooked but equally crucial to modern medicine: blood gas analyzers.
These unassuming devices might not be as visually captivating, but their impact on patient care is profound, providing a window into the intricate workings of the lungs and offering vital data for managing critical conditions. The story of the blood gas analyzer is a captivating journey through innovation and evolution, driven by a relentless pursuit of understanding and treating respiratory distress.
for centuries, we understood that the lungs were essential for life, but it wasn’t until the 17th century that Robert Boyle unraveled the secret of air’s life-sustaining properties. Despite groundbreaking advances in understanding lung physiology, extracting precise data about oxygen and carbon dioxide levels in the blood remained a complex and time-consuming endeavor. By the 1940s, techniques like the Van Slyke apparatus, perfected by chemist Donald D. Van Slyke in 1917, offered valuable insights into patients with chronic conditions.But for acute emergencies, these methods proved inadequate.
The 1952 polio epidemic that ravaged Copenhagen provided a brutal lesson in the limitations of existing technology. As patients flooded the Blegdam hospital, desperately struggling to breathe, the single iron lung available proved insufficient. Anesthesiologist Bjorn Ibsen, recognizing the dire situation, adapted a breathing technique used for surgical patients – positive pressure ventilation – to provide life support. He and over 1,000 medical students worked tirelessly, hand-ventilating patients around the clock.This heroic effort not only saved countless lives but also ushered in the era of modern intensive care, demonstrating the critical need for rapid and precise monitoring of patients’ lungs.
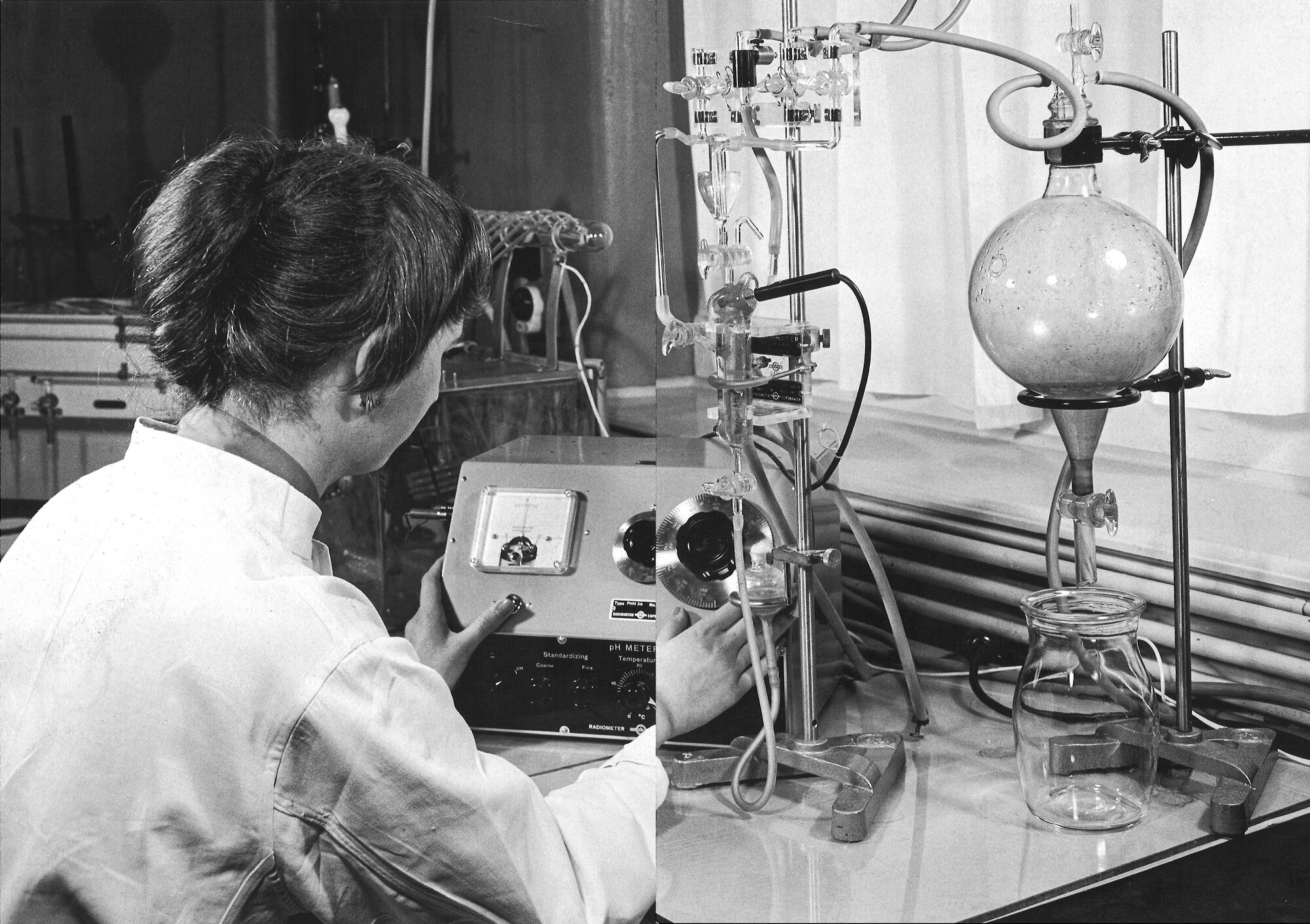
Working behind the scenes, clinical chemist Poul Astrup at the Blegdam made a crucial contribution. By recognizing the link between blood pH and carbon dioxide levels, he could quickly determine the CO2 content in a patient’s blood using his innovative glass electrode. this breakthrough enabled doctors to understand and treat respiratory distress with unprecedented speed and accuracy. Astrup, using a combination of his own pH electrode design and a commercial analyzer from Danish firm Radiometer – a company born from the booming radio industry of the 1920s – created the first blood gas analyzer, a device forever changing the landscape of critical care.
The story of the blood gas analyzer is a testament to the power of innovation, driven by a desire to improve patient outcomes. These unassuming machines, often overshadowed by their flashier counterparts, stand as silent heroes, quietly contributing to the countless lives saved and improved every day.
From Polio Pandemic to Pandemic Powerhouse: The Rise of Blood Gas Analysis
In the 1950s, a polio epidemic gripped Copenhagen, prompting a race to save lives. Facing this medical crisis, pioneering physiologist Astrup, along with a team of researchers, devised a rudimentary device to quickly analyze the blood’s pH levels and carbon dioxide content. This innovation was pivotal, laying the groundwork for a revolutionary medical instrument that would change the landscape of intensive care: the blood gas analyzer.
Building on Astrup’s work, Radiometer, a Danish company known for its scientific instruments, partnered to develop the Astrup-Micro-Equipment 1 (AME1). This device, with its unassuming design and essential functionality, earned the nickname “Blodbil” – the “blood car” – in Danish hospitals.The AME1 introduced a radical concept: bringing laboratory-level precision directly to patients’ bedsides. Its wheels allowed for unprecedented mobility, transforming the hospital ward into a dynamic space where rapid medical interventions became possible.
“I have a vivid recollection of that Saturday in August of 1964,” recalled Dr. Thomas Petty, a pioneer in respiratory medicine, “when I finally mastered the Clark PO2 and Severinghaus CO2 electrodes, which came with my new Radiometer blood gas equipment.”
The AME1 empowered physicians to monitor patients’ oxygen and carbon dioxide levels with unprecedented accuracy. This capability revolutionized the understanding and treatment of lung disorders.Doctors could now directly observe the effects of their interventions, be it oxygen therapy or mechanical ventilation, on the patient’s blood gas levels. This feedback loop fueled faster and more precise treatment decisions, ushering in a new era of therapeutic experimentation.
The impact of the AME1 extended far beyond individual patients. The ability to rapidly analyze blood gases fueled the discovery of Acute Respiratory Distress Syndrome (ARDS), a life-threatening lung condition often requiring mechanical ventilation. The defining feature of ARDS, as characterized by Petty and his team in 1967, was a positive response to aggressive ventilation. Simply put, if a patient’s oxygen levels improved with high-pressure air delivered to their lungs, they were diagnosed with ARDS.
this close association between diagnosis and treatment, fueled by the AME1’s abilities, highlighted the transformative power of technology in shaping medical understanding. The blood gas analyzer did more than just provide measurements; it blurred the lines between diagnosis and intervention, transforming the hospital ward into a dynamic laboratory for medical breakthroughs.
The legacy of the AME1 and its impact on Radiometer are undeniable. Radiometer, once known primarily for scientific instruments, shifted its focus to the more lucrative medical devices market, becoming a global leader in blood gas analysis. The success of the AME1 marked a broader trend, with non-medical industries recognizing the immense potential of the burgeoning field of postwar medicine.
ARDS, a condition once shrouded in mystery, is now a familiar presence in hospitals worldwide, its diagnosis often signaling the need for mechanical ventilation. The AME1’s enduring impact was especially evident during the early stages of the COVID-19 pandemic, where a diagnosis of ARDS frequently meant a patient’s life depended on a ventilator, underscoring the profound relationship between this life-saving technology and the global fight against respiratory illnesses.
The debate surrounding the management of oxygen levels in critically ill COVID-19 patients remains a sensitive one for intensive care physicians. While modern oxygen sensors provide a clear picture of a patient’s oxygen saturation, even if their lungs appear to function normally, the emphasis on blood gas levels – a legacy rooted in the influence of Radiometer and the AME1 device – lead to unnecessary ventilation for many patients. This overreliance on a single metric, experts suggest, may have inadvertently contributed to a higher number of fatalities.
The AME1 stands as a powerful symbol of the complex landscape of medical technology. It represents a confluence of remarkable innovation, the mundane realities of technological ecosystems, and, perhaps, the risk of unintended harm. Understanding the history of such medical artifacts, thus, becomes a multifaceted endeavor, interwoven with the strands of medical history, technological evolution, and the practical realities of patient care.
What are some key challenges that Dr. Astrup and his team faced in developing the AME1?
From Polio pandemic to Pandemic Powerhouse: An Interview with Dr. Anna Larson, Radiometer Historian
Dr. Anna Larson, a historian specializing in the intersection of technology and medicine at Radiometer, recently sat down with us to discuss the fascinating history of the blood gas analyzer. Her insights illuminate not only the technical evolution of this vital medical tool but also its profound impact on patient care.
How did the need for a rapid and accurate method to measure blood gases emerge?
“The 1952 polio epidemic in Copenhagen was a turning point. It highlighted the critical need for immediate, precise information about patients’ respiratory status. Existing methods were too slow and cumbersome, especially in a crisis. The Blegdam hospital’s desperate need during those months fueled the growth of new technologies. Poul Astrup’s groundbreaking understanding of the link between blood pH and CO2 levels, coupled with the ingenuity of Dr. Bjorn Ibsen’s adaptation of positive pressure ventilation, set the stage for a truly revolutionary device.
Tell us about the creation of the AME1. What made it so groundbreaking?
“The AME1, or Astrup-Micro-Equipment 1, was a marvel of its time. It was designed in collaboration with Astrup and Radiometer, who recognized the immense potential of his work.What truly set it apart was its portability. Before, blood gas analysis was a laboratory procedure, inaccessible to critically ill patients. The AME1 brought that expertise directly to the bedside. Doctors could now make timely decisions based on real-time data, which was a game-changer in managing respiratory distress,” Dr. Larson explained.
How did the AME1 impact the understanding and treatment of lung conditions?
“The AME1 revolutionized the understanding of respiratory illnesses. It allowed doctors to directly observe the effects of treatments, figure out what was working and what wasn’t, and adjust accordingly. The discovery of Acute Respiratory Distress Syndrome (ARDS) directly stemmed from the insights gained through using the AME1. Its ability to differentiate between different forms of respiratory distress, enabled more targeted and effective interventions.”
What is the lasting legacy of the AME1?
“The AME1’s legacy is vast. Radiometer became a world leader in blood gas analysis, shaping the course of modern critical care. But perhaps the most profound impact is its ongoing influence on clinical practice. To this day, doctors rely on these measurements to understand and manage lung function. The AME1’s evolution into even more elegant devices has propelled the development of personalized medicine, tailored to each patient’s unique respiratory needs.
Looking Ahead: How has the field of blood gas analysis evolved since the AME1’s debut?
“Today, we have technology that provides instant, accurate oxygen and carbon dioxide readings, even through wearable sensors. However,” Dr. larson cautions, “we must remember the lessons learned from the AME1 era. Continued research and careful evaluation are crucial to ensure that we avoid overreliance on any single metric and strive for a holistic approach to patient care.
The AME1 serves as a powerful reminder that medical innovation is not just about technological advancements; its about understanding how these tools can best serve patients and improve their lives.