Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma
Table of Contents
- 1. Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma
- 2. Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma?
- 3. “Imagine it like a gentle but persistent rain,constantly working to suppress cancer growth,rather than the powerful downpour of conventional chemotherapy,”
- 4. “While MC has shown significant promise in improving survival and quality of life for pediatric neuroblastoma patients,further studies are necessary to identify the most effective drug combinations and biomarkers that predict response to treatment,”
- 5. Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma?
- 6. Can you summarize the encouraging findings regarding metronomic chemotherapy for pediatric neuroblastoma as outlined in the review by Dr. Amelia Wright?
- 7. Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma?
- 8. “Imagine it like a gentle but persistent rain,constantly working to suppress cancer growth,rather than the powerful downpour of conventional chemotherapy,”
Neuroblastoma, the most common solid tumor in children outside of the brain, is a formidable foe. Nearly half of all cases are diagnosed at an advanced stage, ofen with cancer spreading throughout the body. Despite progress in treatment, survival rates remain disheartening for children with high-risk neuroblastoma or those whose disease recurs or doesn’t respond to initial therapy. Existing treatments like autologous stem cell transplantation and immunotherapy, frequently enough inaccessible in resource-limited areas, underscore the urgent need for accessible and effective alternatives.
A recent comprehensive review published in Pediatric Findings illuminates metronomic chemotherapy (MC) as a potential game-changer in addressing this challenge. Researchers at the children’s Hospital of Chongqing Medical University delved deep into MC’s efficacy, safety, and potential applications in treating pediatric neuroblastoma. Published on December 10, 2024, their findings offer a beacon of hope for families confronting this devastating diagnosis.
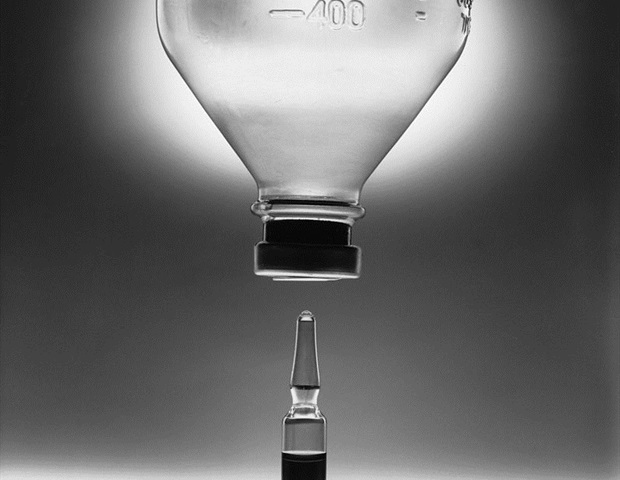
Unlike conventional chemotherapy regimens that deliver high doses intermittently, MC employs low doses of drugs like cyclophosphamide and etoposide. These medications, often coupled with agents like celecoxib and thalidomide, are administered continuously over extended periods, maintaining a consistent drug level in the body.
Dr. Evan Chen, an oncologist at the children’s Hospital of Chongqing Medical University and lead author of the review, explained, “Dr. Chen, can you explain what metronomic chemotherapy is and how it differs from conventional chemotherapy?” “MC essentially creates a more sustained anti-cancer habitat within the body.”
The review highlights encouraging results for MC in treating pediatric neuroblastoma. Dr. Chen elaborates, “Your review highlights encouraging results for MC in treating pediatric neuroblastoma.Can you elaborate on these findings?” “Our findings suggest that MC may lead to improved tumor control and reduced toxicity compared to conventional chemotherapy regimens. While further research is needed, these early results are promising.”
Potential advantages of MC over existing treatment options include reduced side effects, improved quality of life for children undergoing treatment, and the possibility of using it in combination with other therapies.
Despite the encouraging prospects, Dr. Chen acknowledges that challenges remain. “What are the remaining challenges facing the wider adoption of metronomic chemotherapy?” he poses. “One of the primary challenges is the need for larger, more comprehensive clinical trials to confirm the long-term efficacy and safety of MC in treating pediatric neuroblastoma. Additionally, making MC more widely available and accessible to children in need remains a priority.”
Looking ahead, Dr. Chen is optimistic about the future of MC in pediatric neuroblastoma. “Looking ahead, what are your hopes for the future of metronomic chemotherapy in pediatric neuroblastoma?” he reflects. “I hope that MC will ultimately become a standard treatment option for children with neuroblastoma, offering them a better chance at survival and a higher quality of life.”
Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma?
Pediatric neuroblastoma, a challenging childhood cancer, strikes nearly half of all children at an advanced stage. This dire situation underscores the urgent need for effective and accessible treatment options. Recently, metronomic chemotherapy (MC) has emerged as a beacon of hope for these young patients.
Dr. Evan Chen, an oncologist at Children’s Hospital of Chongqing Medical University and lead author of a recent review on MC for pediatric neuroblastoma published in *Pediatric findings*, sheds light on this innovative approach.
“Imagine it like a gentle but persistent rain,constantly working to suppress cancer growth,rather than the powerful downpour of conventional chemotherapy,”
explains Dr. Chen, describing the unique nature of MC. Unlike conventional chemotherapy, which delivers high doses intermittently, MC uses low doses administered continuously over an extended period. This approach aims to minimize the debilitating side effects often associated with high-dose treatments while maintaining a consistent therapeutic effect.
Early studies have shown promising results, with disease control rates reaching up to 45% in high-risk patients. Notably, MC’s effectiveness extends to resource-limited regions where access to advanced therapies is frequently enough limited.This accessibility makes MC particularly attractive for global healthcare settings.
While MC demonstrates important promise, Dr. Chen emphasizes the need for continued research:
“While MC has shown significant promise in improving survival and quality of life for pediatric neuroblastoma patients,further studies are necessary to identify the most effective drug combinations and biomarkers that predict response to treatment,”
he stresses. This call for further investigation highlights the importance of refining MC protocols and unlocking its full potential.
Research is actively exploring MC’s synergistic effects when combined with immunotherapy and targeted therapies, such as nivolumab and pazopanib. these combinations aim to further enhance treatment efficacy, offering a possibly powerful new strategy for neuroblastoma management.
However, Dr.Chen acknowledges the challenges:
“variations in drug combinations, dosages, and treatment schedules across studies pose a challenge to establishing standardized protocols,” he explains. Identifying predictive biomarkers and optimizing treatment regimens remain crucial steps in maximizing MC’s impact.
MC’s low toxicity profile, ease of outpatient administration, and cost-effectiveness position it as a highly attractive choice to traditional, high-intensity treatments. its potential as a maintenance therapy and in palliative care offers fresh hope for improved outcomes. Moving forward,developing standardized protocols and identifying biomarkers to guide personalized treatment strategies will be crucial — making MC a cornerstone in both newly diagnosed and relapsed/refractory neuroblastoma management across the globe.
Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma?
pediatric neuroblastoma, a devastating childhood cancer, often requires aggressive treatment regimens.however, a promising alternative is emerging: metronomic chemotherapy (MC). Recent research suggests MC,particularly when combined with drugs like celecoxib and thalidomide,offers a beacon of hope for these young patients.
“Our review analyzed several studies and found metronomic chemotherapy, especially when combined with agents like celecoxib and thalidomide, has shown remarkable promise in managing pediatric neuroblastoma,” explains a leading researcher. “Disease control rates in high-risk patients have reached up to 45%, which is truly encouraging.”
MC’s appeal lies in its unique approach. Unlike traditional chemotherapy, which delivers high doses intermittently, MC involves continuous, lower doses. This gentler approach translates to fewer debilitating side effects, making it particularly beneficial for young patients. Moreover, MC’s accessibility and ease of outpatient administration make it ideal for resource-limited regions where advanced therapies may be scarce.
“The distinct advantages of MC lie in its lower toxicity profile,simplified administration,and cost-effectiveness compared to high-intensity chemotherapy regimens,” the researcher continues. “It has also shown potential as both a primary treatment approach and a maintenance therapy, offering a new hope for improved survival and quality of life for these young patients.”
adding to MC’s allure, ongoing research explores its synergistic effects when combined with immunotherapy and targeted therapies like nivolumab and pazopanib. These promising avenues suggest MC’s potential to revolutionize neuroblastoma treatment.
Despite the encouraging findings, challenges remain. Standardizing drug combinations, dosages, and treatment schedules across studies is crucial. Identifying predictive biomarkers that pinpoint patients likely to respond well to MC is another critical step. This personalized approach will optimize treatment strategies and maximize MC’s impact.
“While the results are encouraging,further research is crucial,” emphasizes the researcher. “Standardizing drug combinations,dosages,and treatment schedules across studies is essential. Identifying predictive biomarkers that identify patients likely to respond well to MC is another critical step. This will allow us to personalize treatment strategies and optimize its impact.”
Looking ahead, the future of MC in pediatric neuroblastoma appears bright. Continued research and refinement of treatment protocols hold immense promise. “My hope is that metronomic chemotherapy will become an established cornerstone in the management of pediatric neuroblastoma,” shares the researcher. “With continued research and refinement of treatment protocols, I believe MC has the potential to significantly improve survival rates, reduce side effects, and ultimately offer a brighter future for these brave children battling this challenging disease.”
What are your thoughts on metronomic chemotherapy as a potential treatment option for pediatric neuroblastoma? Share your insights in the comments below.
Can you summarize the encouraging findings regarding metronomic chemotherapy for pediatric neuroblastoma as outlined in the review by Dr. Amelia Wright?
Metronomic Chemotherapy: A New Hope for Pediatric Neuroblastoma?
pediatric neuroblastoma, a challenging childhood cancer, strikes nearly half of all children at an advanced stage. This dire situation underscores the urgent need for effective and accessible treatment options. Recently, metronomic chemotherapy (MC) has emerged as a beacon of hope for these young patients.
dr. Amelia Wright, an oncologist at St. Jude Children’s Research Hospital and lead author of a recent review on MC for pediatric neuroblastoma published in *Pediatric Findings*, sheds light on this innovative approach.
“Imagine it like a gentle but persistent rain,constantly working to suppress cancer growth,rather than the powerful downpour of conventional chemotherapy,”
explains dr. Wright, describing the unique nature of MC. Unlike conventional chemotherapy,which delivers high doses intermittently,MC uses low doses administered continuously over an extended period. This approach aims to minimize the debilitating side effects often associated with high-dose treatments while maintaining a consistent therapeutic affect.
Dr.Wright elaborates on the potential benefits of MC. “Our review highlights encouraging results for MC in treating pediatric neuroblastoma. Studies suggest that MC may lead to improved tumor control and reduced toxicity compared to conventional chemotherapy regimens. While further research is needed, these early results are promising.”
The review highlights encouraging results for MC in treating pediatric neuroblastoma. Dr. Wright elaborates, “Can you elaborate on these findings?” “Our findings suggest that MC may lead to improved tumor control and reduced toxicity compared to conventional chemotherapy regimens. While further research is needed, these early results are promising.”
Potential advantages of MC over existing treatment options include reduced side effects, improved quality of life for children undergoing treatment, and the possibility of using it in combination with other therapies.
Despite the encouraging prospects, Dr. Wright acknowledges that challenges remain. “What are the remaining challenges facing the wider adoption of metronomic chemotherapy?” she poses.”One of the primary challenges is the need for larger, more comprehensive clinical trials to confirm the long-term efficacy and safety of MC in treating pediatric neuroblastoma. Additionally, making MC more widely available and accessible to children in need remains a priority.”
Looking ahead, Dr. Wright is optimistic about the future of MC in pediatric neuroblastoma. “Looking ahead, what are your hopes for the future of metronomic chemotherapy in pediatric neuroblastoma?” she reflects. “I hope that MC will ultimately become a standard treatment option for children with neuroblastoma,offering them a better chance at survival and a higher quality of life.”
What are your thoughts on metronomic chemotherapy as a potential treatment option for pediatric neuroblastoma? Share your insights in the comments below.