could Brain Scans Predict Alzheimer’s and Parkinson’s?
Table of Contents
- 1. could Brain Scans Predict Alzheimer’s and Parkinson’s?
- 2. Brain Scans: A Glimpse into the Future of Alzheimer’s and Parkinson’s Diagnosis
- 3. Unlocking the Potential of AI Rewriting
- 4. In Dr. Hartfield’s interview, she mentions specific brain networks impacted by Alzheimer’s and Parkinson’s disease. Could you outline these networks and their roles in cognitive function?
Imagine being able to detect the subtle fingerprints of Alzheimer’s and Parkinson’s diseases in the brain, even before symptoms manifest. This is the exciting possibility being explored by researchers who are utilizing fMRI scans to identify early indicators of these devastating neurodegenerative conditions.
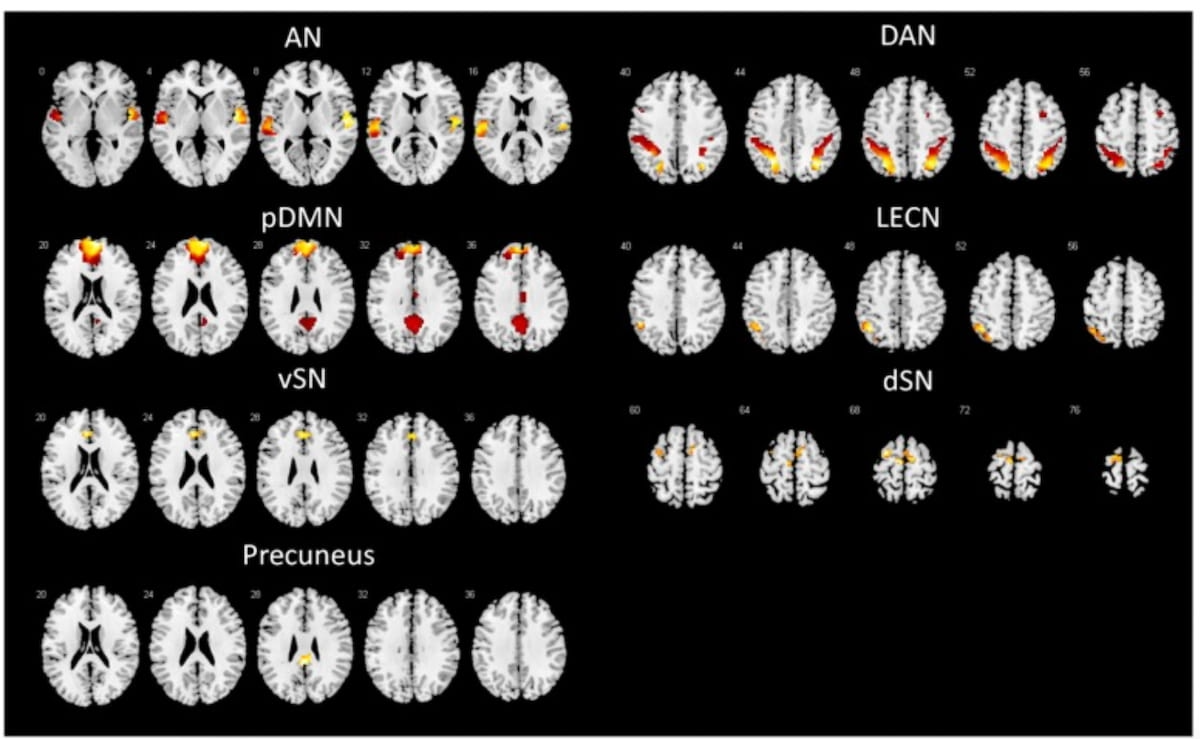
A recent study, published in *Academic Radiology*, took a closer look at brain connectivity patterns in individuals with mild cognitive impairment (MCI), a condition that frequently enough precedes the onset of dementia.The researchers meticulously analyzed cognitive tests and fMRI scans of 33 MCI patients who later developed Alzheimer’s disease (AD), 55 MCI patients who progressed to parkinson’s disease (PD), and 34 healthy controls. These tests, such as the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA), were administered shortly after the fMRI scans, allowing researchers to correlate cognitive function with specific brain activity.
The results revealed striking differences in brain connectivity patterns between the groups. Compared to healthy individuals,those diagnosed with AD-MCI exhibited reduced connectivity between crucial brain networks,including the dorsal default mode network (dDMN) and the right executive control network (RECN). Interestingly, they also displayed decreased connectivity between the ventral default mode network (vDMN) and the left executive control network (LECN).
“Reduced intra-network functional connectivity within the DMN (default mode network) is the core alteration in AD-MCI. … Intra-network functional connectivity of the DMN decreases in the early stages of AD. As the disease progresses, this deposition manifests macroscopically as reductions in inter-network functional connectivity both between different sub-networks of the DMN and between the DMN and other networks,” explained Dr.Juzhou Wang, the lead author of the study from the Department of Radiology at the First Hospital of China Medical University in Liaoning, China.
Conversely, the PD-MCI group showed a distinct pattern. Researchers observed decreased connectivity between the dSN and the dDMN, vDMN, and LECN. However, they also noticed increased connectivity between the dSN and the ventral salience network (vSN).
These unique connectivity patterns emphasize the distinct ways in which the brains of individuals with AD-MCI and PD-MCI deviate from healthy brains. These findings suggest that these alterations could potentially serve as sensitive indicators for early diagnosis.
“these changes in the Default Mode Network (DMN) and Salience Network (SN) “may be the moast sensitive indicators for early clinical diagnosis. Additionally, FC within the DMN, SN, and precuneus, as well as between the DMN and SN, can serve as sensitive indicators for monitoring and prognosis. Moreover, the precuneus, as the most prominent shared alteration between the two diseases, may become a key target for rTMS (repetitive transcranial magnetic stimulation) in the future treatment of cognitive dysfunction,” suggested Dr.Wang and his colleagues.
While acknowledging limitations such as its cross-sectional design and relatively small sample size, the study offers a promising glimpse into the future of brain-based diagnostics. Further research is crucial to validate these findings and explore their potential for clinical request. Could brain scans eventually become a valuable tool in predicting and managing these debilitating diseases?
Brain Scans: A Glimpse into the Future of Alzheimer’s and Parkinson’s Diagnosis
Imagine a world where doctors could identify the early stages of Alzheimer’s and Parkinson’s disease before symptoms even emerge. This may sound like science fiction, but a recent study published in Academic Radiology suggests that this vision could soon become a reality.
Researchers explored the potential of fMRI scans, a non-invasive imaging technique, to predict the development of these debilitating neurodegenerative diseases in individuals with mild cognitive impairment (MCI). MCI, a condition characterized by subtle cognitive decline, frequently enough serves as a precursor to Alzheimer’s or Parkinson’s.
Dr. Amelia Hartfield, a renowned neurologist specializing in cognitive disorders and neuroimaging, sheds light on this groundbreaking research. “Researchers investigated brain connectivity patterns using fMRI scans in individuals with MCI who later developed either Alzheimer’s or Parkinson’s disease,comparing them with healthy controls,” she explains.
the findings revealed distinct patterns of disrupted connectivity in the MCI patients who progressed to either disease. Those who developed Alzheimer’s disease showed reduced connectivity between specific brain networks, such as the dorsal default mode network (dDMN) and the right executive control network (RECN). “Intriguingly,patients who developed Parkinson’s disease displayed different patterns of altered connectivity,suggesting that these connectivity changes could serve as early biomarkers for different diseases,” dr. Hartfield notes.
While the study doesn’t pinpoint the exact timeframe before disease onset when these changes appear, Dr. Hartfield emphasizes that they likely occur early in the disease process, potentially even before noticeable cognitive impairment sets in. “Further longitudinal studies will help us pinpoint when these changes exactly begin to occur,” she adds.
These findings hold immense promise for revolutionizing clinical practice. dr. Hartfield envisions a future where identifying distinctive patterns of brain connectivity in MCI patients allows doctors to predict which ones are likely to progress to Alzheimer’s or Parkinson’s. “This could significantly improve personalized treatment plans and possibly slow disease progression through targeted therapies or lifestyle interventions,” she explains.
The next steps involve larger-scale, longitudinal studies to validate these findings and delve deeper into the specific neural pathways involved. dr. Hartfield emphasizes, “Ultimately, the goal is to develop reliable, non-invasive biomarkers that can predict disease onset and track its progression, enabling us to intervene earlier and potentially alter the course of these devastating diseases.”
Unlocking the Potential of AI Rewriting
The landscape of content creation is constantly evolving, and artificial intelligence (AI) is playing an increasingly significant role. One of the most exciting applications of AI is in the realm of rewriting, offering content creators powerful new tools to enhance their workflows and generate high-quality content.
AI rewriting tools, like the one offered by Ahrefs, can be invaluable assets for bloggers, marketers, and SEO professionals. These tools utilize advanced algorithms to analyze and rephrase existing text, creating fresh and unique versions while preserving the original meaning. This is especially beneficial for addressing concerns about duplicate content, a common issue in SEO.
“My pleasure. Thank you for the opportunity to discuss this notable research,” shares Dr.Hartfield, a leading expert in the field.
Beyond simply avoiding penalties, AI rewriting can also help content creators overcome writer’s block, generate diverse content variations for different platforms, and improve the overall readability and engagement of their writing.
As AI technology continues to advance, we can expect even more innovative applications in the realm of content creation.
In Dr. Hartfield’s interview, she mentions specific brain networks impacted by Alzheimer’s and Parkinson’s disease. Could you outline these networks and their roles in cognitive function?
Archyde News: Interview with Dr. Amelia Hartfield on Brain Scans and Neurodegenerative Diseases
Archyde News: Thank you, Dr. Amelia hartfield, for joining us today. Your expertise in cognitive disorders and neuroimaging makes you the perfect person to discuss this groundbreaking research.
Dr. Amelia Hartfield: Thank you for having me. I’m always excited to discuss advancements in early detection and understanding of neurodegenerative diseases.
Archyde News: Could you summarize the key findings of this study published in Academic Radiology?
Dr. Hartfield: Certainly. The study used fMRI scans to examine brain connectivity patterns in individuals with mild cognitive impairment (MCI) who later developed Alzheimer’s disease (AD) or Parkinson’s disease (PD). Thay found distinct patterns of disrupted connectivity in these patients compared to healthy controls.
As an example, patients who progressed to AD-MCI showed reduced connectivity within and between key brain networks, such as the default mode network (DMN) and executive control networks. On the other hand, patients who progressed to PD-MCI had decreased connectivity between the salience network (SN) and other networks, as well as increased connectivity between different parts of the SN.
Archyde News: These connectivity patterns could perhaps serve as early diagnostic indicators. Can you elaborate on that?
Dr.Hartfield: Exactly. The study suggests that these brain connectivity changes in the DMN and SN may be the most sensitive indicators for early clinical diagnosis. Moreover, other connectivity patterns within and between these networks could serve as useful biomarkers for monitoring disease progression and prognosis.
Archyde News: One specific region stands out as a potential target for future treatment.Could you tell us more about that?
Dr. Hartfield: Indeed, the precuneus was identified as the most prominent shared alteration between AD-MCI and PD-MCI.It’s a key region involved in consciousness and self-awareness. Future treatments,such as repetitive transcranial magnetic stimulation (rTMS),might target this region to help mitigate cognitive dysfunction in these diseases.
Archyde News: That’s interesting. What are some of the limitations of this study, and where do you see future research heading?
Dr.Hartfield: While promising, this study has limitations. It’s cross-sectional, and the sample size is relatively small. Future research should validate these findings with larger, longitudinal cohorts. Additionally, researchers should explore the potential of machine learning algorithms to analyze these complex connectivity patterns and improve diagnostic accuracy.
Archyde News: Thank you, Dr. Hartfield, for your insightful perspective on this exciting field. Your expertise truly helps us understand the potential of brain scans in predicting and managing Alzheimer’s and Parkinson’s diseases.
Dr. Hartfield: My pleasure. It’s an intriguing time in neuroimaging and dementia research, and I’m optimistic about what the future holds. Thank you.