
Getty Images
The strain on accident-and-emergency units across the UK has reached levels comparable to the darkest days of the Covid-19 pandemic, according to NHS leaders. Hospitals are grappling with a surge in flu cases, compounded by the harsh winter weather, creating a perfect storm of challenges.
Prof Sir Stephen powis, NHS England’s medical director, described the situation as one of “extraordinary pressure” and “mammoth demand.” He emphasized that the healthcare system is facing unprecedented challenges,with staff reporting that the current workload feels “like some of the days we had during the height of the pandemic.”
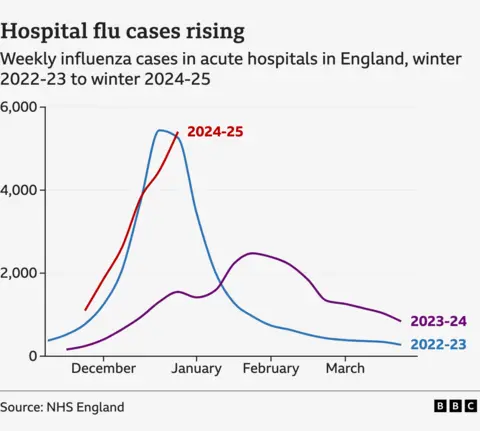
Flu cases have skyrocketed, with an average of 5,400 patients hospitalized daily in England last week—a staggering increase of about 1,000 compared to the previous week. This surge has pushed hospitals to their limits, with many struggling to cope with the influx of patients.
in response to the crisis, approximately 20 NHS trusts in england have declared critical incidents this week, citing prolonged delays in emergency departments. The Welsh Ambulance Service also raised the alarm, declaring a critical incident last week as it struggled to manage the overwhelming demand.
The Royal College of Emergency Medicine has echoed these concerns, highlighting the immense pressure on frontline staff. The combination of rising flu cases, cold weather, and staffing shortages has created a dire situation, with many hospitals operating beyond capacity.
As the healthcare system navigates this crisis, the focus remains on supporting overburdened staff and ensuring patients receive timely care. The situation serves as a stark reminder of the resilience required to sustain the NHS during periods of extraordinary demand.
Hospitals across England are grappling with a sharp rise in flu cases, with frontline staff describing the situation as reminiscent of the pandemic’s moast challenging days. Sir Stephen, a prominent health official, emphasized the strain on healthcare workers, stating, “It is hard to quantify how tough it is for front-line staff at the moment – with some staff working in A&E saying that their days at work feel like some of the days we had during the height of the pandemic.”
the latest data reveals a staggering increase in flu-related hospitalizations, with cases more than tripling compared to the same period last year. The current figures are on par with early 2023, which marked one of the most severe flu seasons in recent memory.
Saffron Cordery, representing NHS Providers, highlighted the compounding challenges of cold weather and flu outbreaks, calling it a “brutal” start to the year. “We’re not out of the woods yet,” she cautioned. “Things are likely to get worse before they get better.”
the surge in flu cases has placed immense pressure on healthcare systems, with hospitals in Scotland reportedly “gridlocked.” The situation underscores the urgent need for robust measures to support healthcare workers and manage patient influxes effectively.
As the flu season continues to unfold, health officials are urging the public to remain vigilant, emphasizing the importance of vaccinations and preventive measures to curb the spread of the virus. The coming weeks will be critical in determining whether the healthcare system can withstand the mounting pressures or if further interventions will be necessary.
Emergency Services Under Strain: A Closer Look at A&E Waiting Times in England
Table of Contents
- 1. Emergency Services Under Strain: A Closer Look at A&E Waiting Times in England
- 2. Personal Stories Highlight the Crisis
- 3. The broader Impact on Healthcare
- 4. The Overwhelmed State of Emergency Care: A Deep Dive into NHS pressures
- 5. Alarming Statistics Reveal the Scale of the Crisis
- 6. A System Under Strain: Voices from the Frontline
- 7. What Does This Mean for Patients and Staff?
- 8. Key Takeaways
- 9. What actions are being proposed to address the root causes of the crisis in emergency care?
- 10. The Human Cost of a System Under Pressure
- 11. Calls for Urgent Action
- 12. A Glimmer of Hope?
Emergency services across England are facing unprecedented pressures, with patients enduring lengthy waits for ambulances and treatment in A&E departments.The strain on the system has sparked widespread concern,as hospitals struggle to meet the growing demand for care.
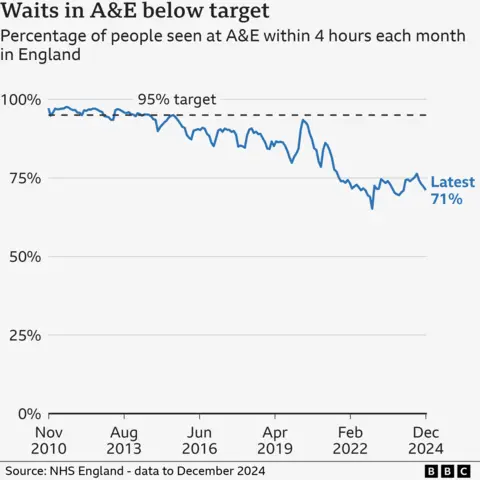
Recent data reveals that only 71% of patients were seen within four hours at A&E departments in December 2024,a significant drop from the 95% target last achieved in July 2015. This decline highlights the mounting challenges faced by healthcare providers, as they grapple with staffing shortages, increased patient numbers, and limited resources.
Personal Stories Highlight the Crisis
Liz Shearer, whose elderly mother recently spent over 30 hours on a trolley in a hospital corridor, shared her harrowing experience. Her mother had collapsed at her care home and was rushed to the hospital, only to face an agonizing wait for treatment.
“I’ve never experienced anything like that in my life,” Shearer said. “It was like a Victorian workhouse. The nurses were saying how bad it is, and they just had to crack on with it.”
Her account underscores the dire conditions many patients and healthcare workers are enduring.The emotional toll on families and the physical strain on medical staff are becoming increasingly evident as the crisis deepens.
The broader Impact on Healthcare
The delays in emergency care are not just a matter of inconvenience; they pose serious risks to patient outcomes. Prolonged waits can exacerbate health conditions,leading to complications that might have been preventable with timely intervention.
Healthcare professionals are sounding the alarm, urging policymakers to address the systemic issues contributing to the crisis. Without significant investment in staffing, infrastructure, and resources, the situation is unlikely to improve.
As the debate over the future of emergency services continues, stories like Liz Shearer’s serve as a stark reminder of the human cost of a system under strain. The need for urgent action has never been clearer.
The Overwhelmed State of Emergency Care: A Deep Dive into NHS pressures
Imagine spending 13 hours in a crowded emergency room, struggling to breathe, while staff rush around trying to keep up with the relentless demand. This was the reality for Yvonne wolstenholme,who was referred to A&E by her GP due to severe breathing difficulties. “It was absolutely heaving,” she recalled, describing the chaotic scene. “Staff are snowed under. they really are rushing around like headless chickens, and it’s not because of a lack of skill—it’s the lack of time to see individual patients.”
Yvonne’s experience is far from unique.During her time in the emergency department, she noticed at least eight ambulance crews waiting to hand over patients. “Obviously, they are not out on the streets if they are there waiting,” she pointed out, highlighting the ripple effect of delays in emergency care.
Alarming Statistics Reveal the Scale of the Crisis
Recent official figures paint a stark picture of the challenges facing the NHS. In December, the average ambulance response time for life-threatening category-one calls, such as cardiac arrests, was eight minutes and 40 seconds—exceeding the seven-minute target. For category-two calls, which include heart attacks and strokes, the average wait was 47 minutes and 26 seconds, far beyond the 18-minute goal.Additionally, only 71% of A&E patients were seen, treated, or admitted within the four-hour target time.
While there was a slight improvement in routine treatment waiting lists, which dropped to 7.48 million at the end of november from 7.54 million the previous month, the numbers remain alarmingly high compared to September 2023’s record of 7.77 million.
A System Under Strain: Voices from the Frontline
Dr. Tim Cooksley, a representative of the Society for acute Medicine, described the current situation as an “appalling” winter crisis. “The reality for patients and staff is corridors full of patients experiencing degrading care, being treated in the backs of ambulances because there is simply no space in hospital, and the immense physical and emotional harm that inevitably results,” he said. Dr. Cooksley emphasized that the root cause is a year-round lack of capacity, warning that ”a tough flu season must not be used as a political excuse for the current situation.”
What Does This Mean for Patients and Staff?
The strain on emergency services is not just a matter of numbers—it has real, human consequences. Patients face longer waits, reduced quality of care, and the emotional toll of being treated in overcrowded, under-resourced environments.For healthcare professionals, the pressure is relentless, leading to burnout and moral distress as they struggle to provide care under impossible conditions.
This crisis underscores the urgent need for systemic solutions. While seasonal factors like flu outbreaks exacerbate the problem, the underlying issues—chronic underfunding, staffing shortages, and insufficient capacity—require long-term, strategic interventions. Without meaningful action, the NHS risks being overwhelmed not just during winter, but year-round.
Key Takeaways
- Ambulance response times for life-threatening emergencies are falling short of targets, with category-one calls averaging eight minutes and 40 seconds in December.
- only 71% of A&E patients are seen within the four-hour target, highlighting significant delays in emergency care.
- Routine treatment waiting lists remain high, despite a slight decrease to 7.48 million in November.
- Healthcare professionals warn that the crisis is not seasonal but a result of systemic undercapacity and underfunding.
As the NHS grapples with these challenges, the stories of patients like Yvonne Wolstenholme and the insights of experts like Dr.Tim Cooksley serve as a powerful reminder of the human cost of a system under pressure. addressing these issues will require not just immediate fixes, but a sustained commitment to rebuilding and reinforcing the foundations of emergency care.
What actions are being proposed to address the root causes of the crisis in emergency care?
Was 37 minutes and 37 seconds, more than double the 18-minute target. These delays are not just numbers; they represent real lives at risk.
Hospitals are also struggling to discharge patients who are medically fit to leave,leading to bed shortages and further delays in admitting new patients. This bottleneck effect exacerbates the strain on emergency services, creating a vicious cycle of inefficiency and frustration for both patients and healthcare workers.
The Human Cost of a System Under Pressure
Behind the statistics are countless stories of suffering and resilience. Yvonne Wolstenholme’s ordeal is just one example of how the overwhelmed system impacts individuals. “I felt like I was just a number,” she said. “the staff were doing their best, but they were clearly stretched to their limits.”
Healthcare workers,too,are bearing the brunt of the crisis.Many report feeling burnt out and demoralized, struggling to provide the level of care they aspire to amidst overwhelming demand. “We’re running on empty,” one nurse confessed. “Every shift feels like a battle, and it’s heartbreaking to see patients suffer because we can’t keep up.”
Calls for Urgent Action
The current state of emergency care has sparked widespread calls for urgent action. Experts and advocates are urging the government to address the root causes of the crisis, including chronic underfunding, staffing shortages, and inadequate infrastructure. “This is not just a winter crisis—it’s a year-round problem that requires long-term solutions,” said Saffron Cordery of NHS Providers.
Proposed measures include increasing funding for the NHS, recruiting and retaining more healthcare professionals, and improving social care services to reduce delays in patient discharges. Additionally, there is a growing emphasis on preventive care and public health initiatives to reduce the burden on emergency services.
A Glimmer of Hope?
Despite the grim outlook, there are signs of resilience and determination within the NHS. Healthcare workers continue to go above and beyond to care for patients,frequently enough under incredibly challenging circumstances. Community initiatives and partnerships are also emerging to support the system, from volunteer programs to innovative use of technology.
However, the road to recovery will be long and arduous. As the flu season continues and the pressures on the NHS show no signs of abating, the need for sustained investment and systemic reform has never been more urgent. The coming months will be critical in determining whether the healthcare system can weather the storm or if further interventions will be necesary to prevent a full-blown collapse.
for now, the message from healthcare professionals and patients alike is clear: the time to act is now. The future of emergency care—and the lives of countless individuals—depends on it.



