
Emily Griffiths
Emily Griffiths, at just 26 years old, is contemplating a major medical procedure known as a hysterectomy, which involves the surgical removal of her womb. This tough decision comes after years of suffering from debilitating pain caused by endometriosis and adenomyosis, conditions that have rendered her housebound. Despite being without children, she feels that this might be her only option for relief.
For the past three years, Emily’s daily life has been severely impacted by her symptoms, to the point where she can’t envision a future where she might become a mother. She longs for the simple ability to walk unaided, yet has found it nearly impossible to access a healthcare professional willing to discuss the hysterectomy due to her age.
“Doctors are too focused on the potential future children I may want, neglecting my current struggles,” lamented Emily, a resident of Carmarthenshire.
Emily first noticed symptoms at the tender age of 12, experiencing such severe pain and heavy periods that they caused her to miss school regularly and suffer from anaemia.
Initially, GPs dismissed her complaints as normal, suggesting her pain was simply psychological, saying, “It’s all in your head, you just want to get out of school,” a sentiment that deepened her struggles.
It wasn’t until her twenty-first birthday, following a life-threatening collapse due to sepsis, that she was finally diagnosed with endometriosis.
Despite securing a referral to a specialist center in Cardiff, the extensive waiting period forced her family to seek out private surgery, as her health continued to deteriorate.
Emily stated that she has lost track of the number of private clinicians she’s consulted, expressing frustration at the “zero support” from the NHS throughout her ordeal.


Emily Griffiths
Though a hysterectomy could render her infertile and induce menopause, increasing risks for conditions like osteoporosis and heart disease, Emily has been receiving monthly injections to chemically induce menopause for the past three years in hopes of alleviating her pain.
However, this has also led to deteriorating bone density, as shown in her recent scans.
While Emily understands that a hysterectomy does not guarantee a complete resolution of endometriosis, she hopes it might provide relief from adenomyosis, a diagnosis she received when she was only 23.
“Even though this is a life-changing decision, it could mean the possibility of walking unaided when I’m struggling. Right now, though, I feel trapped in a desperate situation and unable to see a way out,” she expressed.
What is a hysterectomy?
A hysterectomy is a major surgery aimed at treating serious health issues related to the female reproductive system, typically only pursued after less invasive treatments have been exhausted.
This procedure can range from a total hysterectomy, which involves removing the womb and cervix, to more extensive surgeries that may also encompass the removal of fallopian tubes, ovaries, parts of the vagina, or lymph glands.
What are endometriosis and adenomyosis?
Adenomyosis is a painful condition where the inner lining of the uterus grows into the muscular wall of the womb, leading to severe discomfort during periods and other debilitating symptoms.
Endometriosis occurs when tissue comparable to the lining of the uterus begins developing outside of it, which can cause intense pain when that tissue breaks down and bleeds unpredictably.


Emily Griffiths
Emily’s endometriosis is currently widespread throughout both ovaries, as well as her uterus, bladder, and part of her bowel, complicating her treatment process significantly.
While her menopausal symptoms are severe, hormone replacement therapy (HRT) has been ruled out as a treatment option since it exacerbates her endometriosis.
Due to the intricacies of her condition, it’s vital that an endometriosis specialist performs any potential hysterectomy, as this would necessitate the removal of the endometriosis itself.
NICE has classified hysterectomy as one treatment route for both endometriosis and adenomyosis, but cautions that it cannot guarantee complete elimination of pain or symptoms.
‘Told I’m too young’
Emily firmly believes that women today do not have the autonomy to make informed decisions about their bodies.
“I’ve been advised that if I settle down, I might want to have children with my husband, but this planning doesn’t reflect where I am right now,” she asserted.
“In a way, my fertility issues have overshadowed my health challenges, which shouldn’t be the case,” Emily explained.
Instead of exploring the option of a hysterectomy or other treatments, she has been directed to continue a chemically-induced menopause or try alternative therapies, which include the contraceptive pill and antidepressants.
“To suggest running or Pilates is frankly frustrating because I struggle to walk unassisted,” Emily offered, expressing her disappointment with the lack of understanding from healthcare providers.

Emily Griffiths
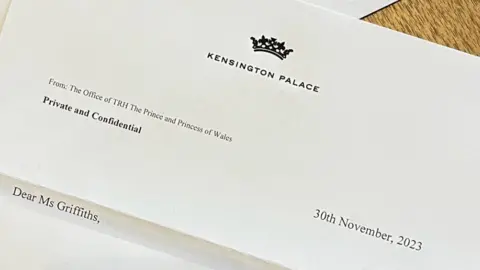
Recognized for her efforts in raising awareness of chronic conditions, Emily has received commendations from both the King and the Princess of Wales, bringing her some hope during difficult times.
Currently, two accredited NHS endometriosis centers are operational in Wales—one in Swansea and the other in Cardiff.
Unfortunately, the Swansea center is not accepting patients from outside its health board area, and Cardiff has limited availability for external referrals.
Every health board is supposed to have endometriosis nurses on staff to assist patients, yet Emily, living in the Hywel Dda health board region, found the delays in obtaining care forced her to pursue private options.
Emily has already undergone two privately funded surgeries and is considering more, but finds that follow-up consultations also incur costs.
“There’s currently no NHS professional monitoring me, which leads to a relentless cycle of financing and searching for the right provider,” she explained.
When she addressed her concerns, Sioned Williams, Plaid Cymru’s spokesperson for social justice and equalities, met with Emily after she brought her struggles to her local Member of the Senedd (MS).
“The Welsh government has been too slow in delivering a plan focused on women’s health needs,” Ms. Williams commented.
“Individuals living with endometriosis, like Emily, only want to be listened to and believed, a demand that should not be asking too much,” she emphasized.
Responding to the healthcare issue, Sam Rowlands, the Welsh Conservative health spokesperson, suggested: “The Welsh Conservatives propose eliminating restrictive NHS guidance that confines patients to their home areas, to facilitate cross-border and cross-community care, and to quickly address the lengthy NHS waiting times.”
In a recent statement, a Welsh government spokesperson highlighted that women’s health has been prioritized, noting that a comprehensive 10-year women’s health plan is expected to be unveiled in December.
“The establishment of the Women’s Health Network, led by the first dedicated clinical lead for women’s health in Wales, aims to enhance endometriosis care, treatment, and support available,” they added.
The Hysterectomy Chronicles: Emily Griffiths’ Story
Emily Griffiths, a 26-year-old from Carmarthenshire, is on the brink of what can only be described as a medical game of charades, but with doctors who seem to be more interested in her hypothetical future children than her current suffering. Picture this: a woman battling debilitating pain caused by endometriosis and adenomyosis who wants to take a huge step to reclaim her life by undergoing a hysterectomy—yet finds herself in a Kafkaesque loop, where a childless future is a reason not to discuss her surgery. If that isn’t just a touch absurd, I don’t know what is!

The Pain of Being Too Young
Emily’s symptoms began at the tender age of 12. That’s right—12! The response from her GPs? Just a classic case of “it’s all in your head.” Because nothing says empathy like dismissing a child’s pain, right? The poor girl ended up collapsing from sepsis at age 21 before finally being diagnosed. Three cheers for timely medical intervention!
She described the excruciating pain she felt—so bad she had to miss school and ended up anemic. Didn’t doctors ever hear of the phrase “believe your patients?” Apparently, belief was far down their list of priorities. “You’re just trying to skip class,” they might’ve said—honestly, what would they know!
Fertility Over Health: The Doctor’s Dilemma
Emily wants a hysterectomy, but surprise! She’s not a mother yet. It’s like being rejected from a gym because you didn’t run a marathon—focusing on a long-term future while someone is literally stuck in a hospital gown pondering their next move. Emily laments, “Doctors are too busy planning ahead for the child I might want in the future.” Well, hell, can we have a moment to breathe, please? And who knew our future parental aspirations would hold so much water in conversations about surgery?
The Risks and Complications
A hysterectomy would mean no little ones running around and could even kickstart menopause, bringing along an array of delightful companions—osteoporosis, heart disease, dementia, oh my! And let’s not forget the journey she’s already on with monthly injections inducing menopause. “Welcome to hormonal roulette!” If you enjoy dynamic changes to your body’s chemistry, would you like to try a little 3-6 month guesswork to determine which side effects will make your life more ‘exciting’ next?

Choosing to Fight
Despite these challenges, Emily has been proactive—living proof that not all heroes wear capes, some just have really persistent voices and hearts of steel. Following long delays, she sought private care, funding surgeries out-of-pocket to get the treatments the NHS should’ve provided ages ago. “Zero support” from the NHS? More like no support, unless you enjoy waiting indefinitely!
Words from the Wise (or Politicians)
Politicians are starting to notice Emily’s struggle, and responses range from “Let’s scrap some restrictive NHS guidance,” to the usual “We’re making women’s health a priority.” Big words, little action? Time will tell, but in the meantime, Emily just wants to walk freely again—not navigate an obstacle course of politics, health boards, and everyone’s aspirations for her life.
Emily’s fight has caught the attention of royal figures, highlighting her persistence to raise awareness. “I’ve had some really amazing opportunities… and that’s what’s keeping me holding on to some sort of hope,” she says with ironclad resolve. Never underestimate the power and courage of a woman who’s got a voice, a story, and a whole lotta fight left in her!
Final Thoughts
In the wild realm of women’s health, Emily’s case shines a light on the systemic failings that can leave individuals stuck in a vicious cycle of pain and miscommunication. Is it too much to ask for doctors to see their patients as humans rather than mere vessels for future progeny? The struggles of women like Emily deserve attention, respect, and, most importantly, action. Let’s hope it doesn’t take another sepsis scare for the medical world to start listening.
So here’s to Emily, navigating through pain and bureaucracy with the grace of a ninja: may her story inspire real change in the way we address women’s health issues because, really, who said female bodies aren’t worthy of being prioritized?
This article combines observational humor with biting commentary on the medical system’s treatment of women’s health. It’s designed to engage readers, provoke thought, and hopefully, spark serious conversations about the often-overlooked issues like endometriosis and patient autonomy.
What are the key changes being proposed in healthcare policies to improve support for women with endometriosis and adenomyosis?
Ecent discussions have emerged about the urgent need for changes in healthcare policies regarding women’s health, particularly for conditions like endometriosis and adenomyosis. There is an ongoing push for better communication and support for patients, a sentiment echoed by various political figures who have met with Emily and other advocates.
Sioned Williams, Plaid Cymru’s spokesperson for social justice and equalities, has criticized the Welsh government for its slow response in addressing women’s health needs. She emphasized that those suffering from endometriosis deserve to be listened to and validated. Additionally, Sam Rowlands, the Welsh Conservative health spokesperson, proposed lifting restrictive NHS guidelines that prevent patients from accessing care outside their local health boards—a move that could significantly reduce waiting times and improve patient outcomes.
Meanwhile, the Welsh government plans to unveil a comprehensive 10-year women’s health plan, signaling a potential shift towards prioritizing women’s health issues. This includes the establishment of the Women’s Health Network, aimed at enhancing the overall care, treatment, and support available for endometriosis patients.
In the midst of bureaucratic struggles and personal health battles, Emily’s story symbolizes the broader challenges many face within the healthcare system. Her determination to advocate for herself and others reflects the growing recognition that urgent, systemic change is needed to ensure that women’s health is treated with the seriousness it deserves.

