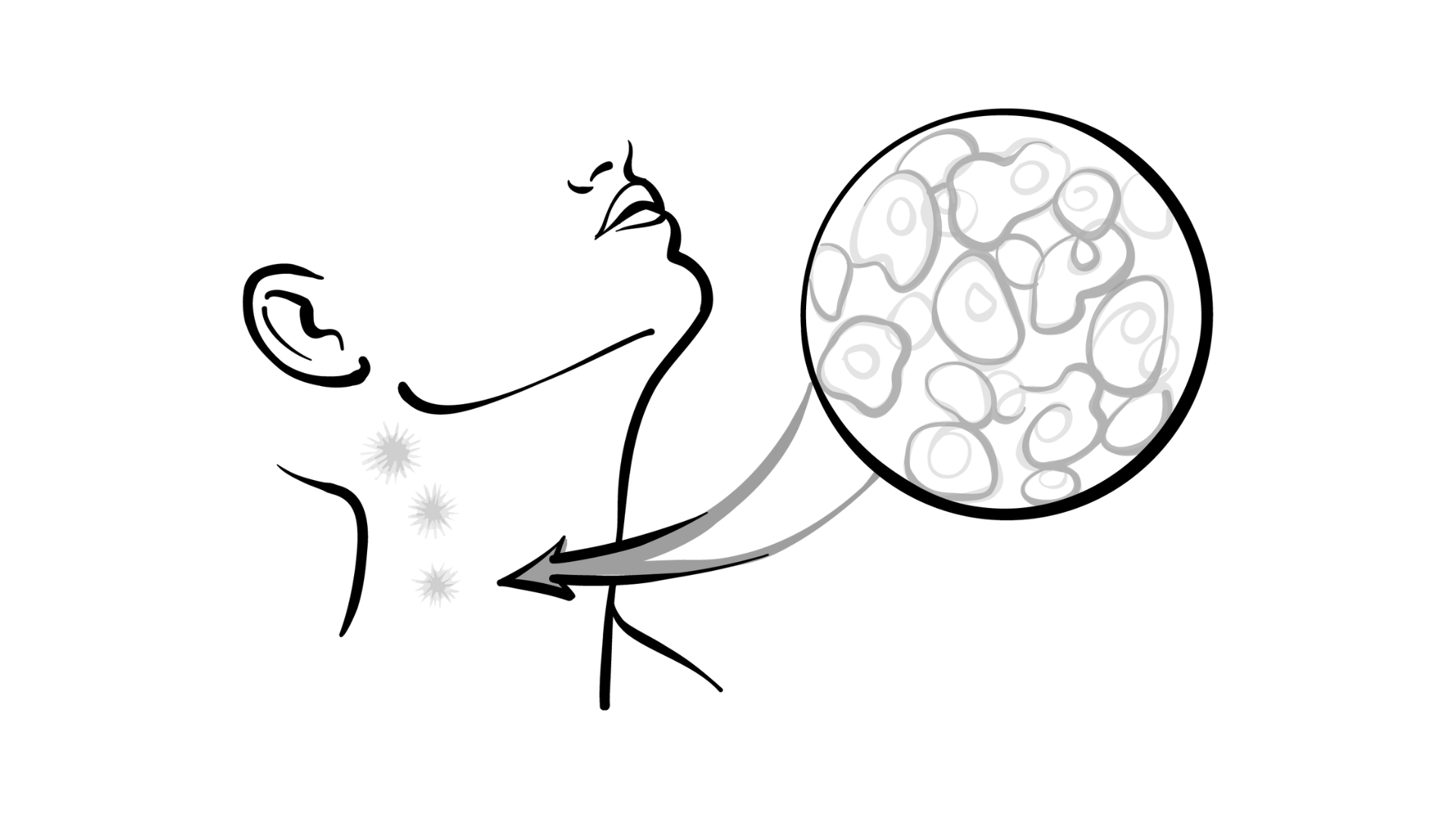
Recent advancements in the treatment landscape for follicular lymphoma (FL) are gaining momentum, largely due to breakthroughs in innovative therapies that show great promise. At the highly regarded 42nd Annual Chemotherapy Foundation Symposium, Erin Mulvey, MD, brought to light the substantial strides being made in managing relapsed or refractory FL. Groundbreaking treatments like Bruton’s tyrosine kinase (BTK) inhibitors and chimeric antigen receptor (CAR) T-cell therapies are already yielding impressive results, significantly enhancing the prospects for patients who have previously failed conventional therapies.
These targeted therapies are revolutionizing the care approach for FL, leading to recent approvals by the FDA and becoming vital components in the therapeutic repertoire. BTK inhibitors precisely target the specific biochemical pathways that lymphoma cells exploit for their survival, while CAR T-cell therapy represents a novel strategy that involves the modification of a patient’s own immune cells to better identify and eliminate cancerous cells. Mulvey, representing Weill Cornell Medical College, stressed the growing array of treatment options available for FL patients, particularly those dealing with challenging disease scenarios, highlighting how these therapies are refining existing treatment frameworks.
With continuous research efforts and the introduction of more pioneering therapies, the trajectory for FL treatment is increasingly leaning toward a more personalized and effective approach. These advancements instill renewed optimism for individuals contending with advanced or resistant FL, potentially facilitating extended remission periods and improved overall survival rates. As these innovative therapies continue to mature, the landscape of FL treatment is set for ongoing enhancements, creating new avenues of hope for patients grappling with the disease.
BTK Inhibitors
In a significant development, the BTK inhibitor zanubrutinib (Brukinsa) has recently received FDA approval for use in combination with obinutuzumab (Gazyva) specifically for patients with FL. This approval was based on compelling data derived from the ROSEWOOD study (NCT03332017), which underlines the efficacy of this combination therapy.
The open-label, multicenter, phase 2 ROSEWOOD trial represented a collective effort involving 217 adult participants with relapsed or refractory FL, all of whom had undergone at least two prior systemic treatment regimens. Patients were assigned in a 2:1 ratio to receive either zanubrutinib at a dosage of 160 mg orally taken twice daily combined with obinutuzumab at 1000 mg administered intravenously, or to receive obinutuzumab alone, following the same dosing regimen. Each treatment cycle lasted 28 days, with obinutuzumab administered on specific days designed to optimize efficacy before transitioning to maintenance therapy every 8 weeks until disease progression, toxicity, or a maximum of two years.
The results were revealing, with an overall response rate (ORR) of 68% in the experimental group compared to 43% in the arm receiving obinutuzumab alone (P = .001). Furthermore, the complete response (CR) rate resembled this trend, showing 39% versus 19%, respectively. Notably, the duration of response (DOR) was not reached in the zanubrutinib arm, contrasting sharply with a median DOR of 26.5 months reported in the obinutuzumab-only cohort (HR, 0.5; P = .001).
Participants in the experimental arm exhibited a median age of 63 (ranging from 31 to 84 years), while those in the obinutuzumab-only group had a median age of 65.5 (ranging from 32 to 88 years). The study included patients from various backgrounds, with 21 participants originating from mainland China in the experimental arm compared to 12 in the obinutuzumab group. Meanwhile, the remaining 124 participants represented a global sample versus 60 patients receiving obinutuzumab alone. Notably, the median prior lines of therapy across all participants amounted to three (spanning two to eleven), with 211 patients demonstrating an ECOG performance score of 0 or 1.
The primary endpoint of this pivotal study was the assessment of ORR as evaluated by independent central review (ICR), while secondary endpoints encompassed the investigator-assessed ORR, DOR, and progression-free survival (PFS) metrics determined through both ICR and investigator assessments, alongside overall survival (OS), CR rate, and cardiac magnetic resonance imaging also reviewed by ICR and the investigator.
In terms of secondary outcomes, the DOR at 18 months stood at 70.9% for the experimental group versus 54.6% for those receiving obinutuzumab alone; and the median PFS was noted to be 27.4 months (95% CI, 16.1-not evaluable [NE]) compared to 11.2 months (95% CI, 6.5-15.7), respectively. When looking at the time to the next treatment intervention, it was noted to be NE (95% CI, 21.1-NE) for the experimental cohort as opposed to 12.1 months (95% CI, 8.3-19.8) for those receiving obinutuzumab alone. Notably, the median OS has yet to be reached in either arm ([95% CI, 31.4-NE] vs [95% CI, 26.8–NE], respectively), as the study was not statistically designed to evaluate differences in OS.
Beyond the requirement of two or more previous lines of therapy, additional criteria included the presence of measurable disease, an ECOG performance status score ranging between 0 to 2, and the absence of any transformation to aggressive B-cell lymphoma.
Mulvey conveyed, “Toxicities were fairly predictable.” She elaborated that “the most common toxicities were hematologic in nature,” with an increase in the incidence of grade 3 or higher adverse events (AEs) linked to the combination therapy. Specifically, thrombocytopenia was reported in 22 patients, while other AEs such as diarrhea, pneumonia, and dyspnea accounted for 4, 14, and 3 cases, respectively. It is worth mentioning that both study arms faced a relatively high rate of grade 3 or higher AEs, yet in the obinutuzumab-only cohort, these occurred in a markedly lower frequency, with figures of 5 for thrombocytopenia, 1 for diarrhea, 3 for pneumonia, and none reported for dyspnea.
CAR T-Cell Therapy
In her discussion, Mulvey also shared insights into the three CAR T-cell therapies currently approved for patient use: axicabtagene ciloleucel (axi-cel; Yescarta), tisagenlecleucel (tisa-cel; Kymriah), and lisocabtagene maraleucel (liso-cel; Breyanzi).
Data stemming from the phase 2 ZUMA-5 trial (NCT03105336) indicated an overwhelming 94% response rate among patients with relapsed FL treated with axi-cel, with a striking 79% achieving a complete response (CR). In addition, 15% of patients recorded a partial response (PR), while 3% experienced stable disease. Remarkably, no patients progressed during the study period. The estimated median PFS across all participants (n=159) was documented at 40.2 months (95% CI, 28.9- not evaluable), and the 36-month estimated PFS rate stood at 54% (95% CI, 45%-63%). Although the median OS has not yet been reached for the cohort, the rate at 36 months is an encouraging 75% (95% CI, 67%-81%). “Bridging chemotherapy was permitted, albeit rarely used, with only 3% receiving it,” Mulvey noted.
For patients who were treated with bendamustine in the six months preceding CAR T-cell intervention, the striking contrast in outcomes was emphasized; the 36-month estimated PFS rate dropped to 25% compared to a robust 70% for those who had no recent exposure to the drug, highlighting the influence of prior therapies on treatment success. Axi-cel exhibited a significant improvement in both PFS and OS when compared against historical control data.
Mulvey added, “This discussion is not intended as a direct comparison, but rather to highlight the distinct characteristics among various CAR T-cell therapies.” Reflecting on findings from the ELARA study involving tisa-cel, she noted an increased risk associated with patients exhibiting higher risk scores, significant tumor bulk, and a greater number of therapy lines than what was seen in other trials. A supplementary concern was the identification of more patients being refractory to axi-cel therapy, particularly among those defined as double refractory to both CD20 antibodies and alkylating agents, resulting in an upward trend for patients who received initial therapy.
References1. Mulvey, E. Expanded options for follicular lymphoma in 2024: a focus on BTKi, CAR-T, and bispecific antibodies. Presented at: Chemotherapy Foundation Symposium: Innovative Cancer Therapy for Tomorrow® Conference; on November 13-15, 2024; New York, New York.2. FDA grants accelerated approval to zanubrutinib for relapsed or refractory follicular lymphoma. FDA. March 7, 2024. Accessed November 13, 2024.
What are the key advancements in follicular lymphoma treatment that Dr. Erin Mulvey discussed during the interview?
**Title: Advancements in Follicular Lymphoma Treatment: An Interview with Dr. Erin Mulvey**
**Interviewer**: Thank you for joining us today, Dr. Erin Mulvey. You recently presented at the 42nd Annual Chemotherapy Foundation Symposium about the latest advancements in treating follicular lymphoma (FL). Can you summarize some of these breakthroughs for our audience?
**Dr. Mulvey**: Certainly! Recent innovations in treatment have really changed the landscape for managing relapsed or refractory follicular lymphoma. We’re seeing promising results with targeted therapies like Bruton’s tyrosine kinase (BTK) inhibitors and chimeric antigen receptor (CAR) T-cell therapies. These treatments allow us to provide more personalized care options to patients who previously faced limited alternatives after conventional therapies failed.
**Interviewer**: That sounds encouraging! Could you tell us a bit about the FDA’s recent approval of BTK inhibitors, particularly zanubrutinib in combination with obinutuzumab?
**Dr. Mulvey**: Of course! Zanubrutinib, also known as Brukinsa, has received FDA approval for use alongside obinutuzumab specifically for patients with FL who have had at least two prior treatments. The ROSEWOOD trial showed remarkable efficacy for this combination, with an overall response rate of 68% compared to just 43% in the group receiving obinutuzumab alone. These statistics highlight how significantly this combination therapy can improve outcomes for patients.
**Interviewer**: Impressive results! Given these advancements, what can you say about CAR T-cell therapies, particularly the findings from the ZUMA-5 trial?
**Dr. Mulvey**: The ZUMA-5 trial yielded fantastic results as well. The CAR T-cell therapy axicabtagene ciloleucel demonstrated a response rate of 94% in patients with relapsed FL, with a remarkable 79% achieving a complete response. Importantly, none of the patients in the study progressed during the trial, and the estimated median progression-free survival was an outstanding 40.2 months. This gives us hope for significantly longer remissions for our patients.
**Interviewer**: Those statistics indeed sound hopeful. As these therapies evolve, how do you see the future of FL treatment changing?
**Dr. Mulvey**: The future of FL treatment is leaning towards more targeted, personalized approaches, which can enhance efficacy and potentially extend survival rates for patients. With continuous research, we anticipate the introduction of even more innovative therapies. This could lead to transformations in how we manage FL, tailoring treatments to the individual characteristics of each patient’s disease.
**Interviewer**: Thank you, Dr. Mulvey, for sharing these exciting advancements. Your insights provide valuable hope for those affected by follicular lymphoma.
**Dr. Mulvey**: Thank you for having me! It’s an exciting time in the field, and I look forward to seeing how these treatments can make a real difference in patients’ lives.