Emerging research indicates that artificial intelligence (AI) segmentation, implemented via multiparametric magnetic resonance imaging (mpMRI), could play a pivotal role in estimating total intraprostatic tumor volume, potentially enhancing the ability to predict metastasis in individuals undergoing treatment for localized prostate cancer (PCa).
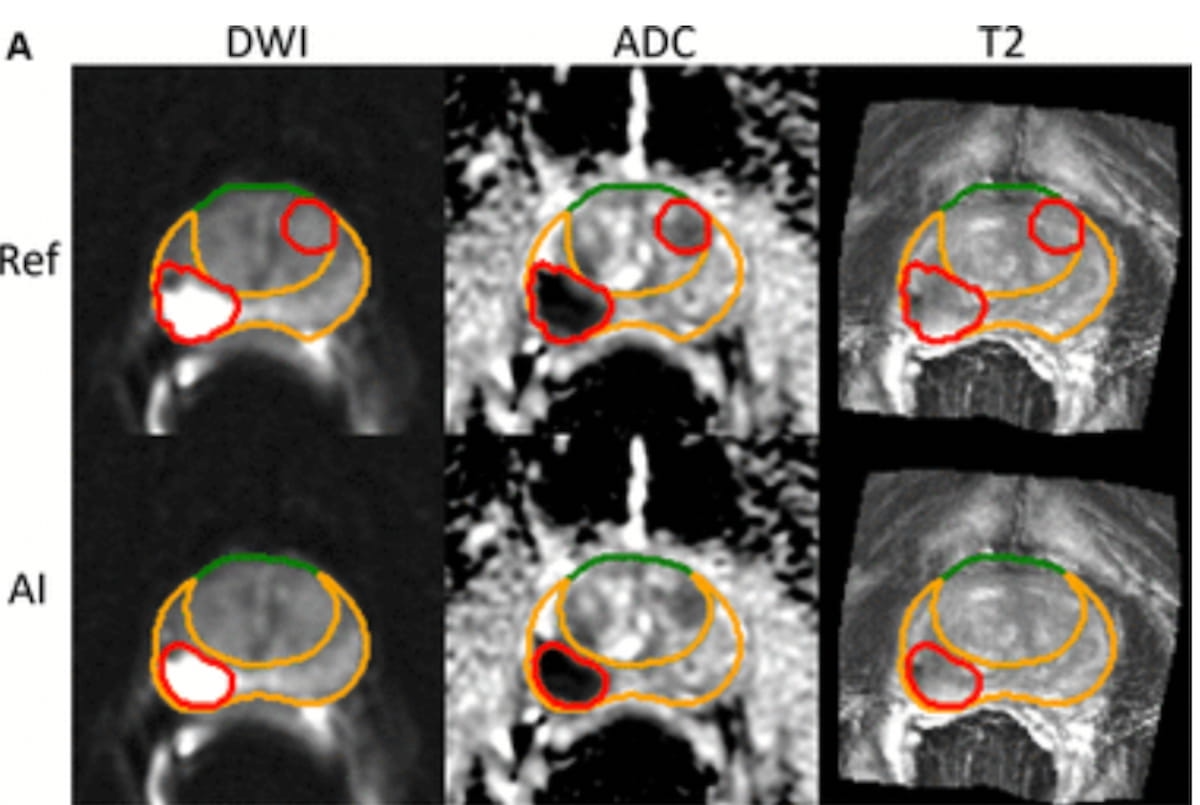
In a significant retrospective study recently published in Radiology, researchers meticulously developed and trained an advanced AI tumor segmentation algorithm aimed at distinguishing Prostate Imaging Reporting and Data System (PI-RADS) lesions scoring from 3 to 5. The authors then conducted a comparative analysis of the total intraprostatic tumor volume obtained through the AI segmentation algorithm (VAI) against the established National Comprehensive Cancer Network (NCCN) risk categorization, aiming to predict metastasis in a cohort of 732 patients who underwent either radical prostatectomy (RP) or radiotherapy (RT) for localized PCa.
The findings revealed that the VAI measurement achieved an impressive 84 percent area under the receiver operating characteristic curve (AUC) for predicting seven-year metastasis within the RT group, surpassing the 74 percent accuracy of the NCCN risk classification. In the cohort undergoing RP, the study uncovered that VAI evaluation displayed a notably higher AUC for predicting metastases over five years, with a score of 89 percent compared to 79 percent for the NCCN system.
“VAI may have been prognostic because it measured the total burden of clinically significant intraprostatic tumors consistently. Although other MRI measures of tumor burden, such as tumor size, PI-RADS scores, and manually delineated tumor volumes, are also prognostic, they are subject to interobserver variability from benign anatomic changes, imaging artifacts, motion artifacts, and variable soft tissue contrast,” wrote lead study author David D. Yang, M.D., who is affiliated with the Department of Radiation Oncology at Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston, and colleagues.
Noting that the application of NCCN risk categorization may exhibit variability due to differences in biopsy sampling strategies and clinical approaches, the authors assert that the VAI model offers enhanced reproducibility and user-friendliness.
“VAI is a highly interpretable entity as a systematic assessment tool for intraprostatic tumors, visible at MRI, that can be easily cross-checked against human-derived tumor volume. Unlike genomic classifiers or digital pathology approaches, no specific retrieval or handling of clinical specimens is required. Additionally, since VAI determination entails an analysis of the entire prostate, under-sampling of aggressive disease is less likely,” emphasized Yang and his colleagues.
Three Key Takeaways
1. AI-assisted tumor volume measurement shows predictive advantage. The AI segmentation model (VAI) demonstrated superior predictive accuracy for metastasis compared to traditional NCCN risk categorization in patients treated with radiotherapy (RT) or radical prostatectomy (RP).
2. Consistent and reproducible measurement. The VAI model may offer a more reproducible method for assessing intraprostatic tumor burden, overcoming limitations associated with other MRI measurements that are prone to variability due to factors like benign anatomic changes and imaging artifacts.
3. Potential to influence treatment decisions. By identifying high-risk patients more accurately, VAI may be a consideration in decision-making for upfront radiotherapy over surgery, especially for patients with aggressive disease who might benefit more from early intervention.
The study authors suggested that utilization of the VAI model may have an impact on the management of PCa.
“For patients with unfavorable-risk disease, a high likelihood of obtaining clinically significant adverse pathologic findings after prostatectomy, for which adjuvant rather than early-salvage RT may be beneficial, may prompt some patients to choose up-front RT instead,” added Yang and colleagues.
Beyond the inherent limitations of a single-center retrospective study, the authors acknowledged that patients in the cohort were diagnosed with PCa prior to the broader use of MRI and ultrasound fusion biopsies. They also cautioned that results obtained with the evaluated AI algorithm in this study may not be applicable with different image acquisition settings or MRI systems from various vendors.
AI and Prostate Cancer: The Future of Tumor Volume Measurement or Just a Flash in the Pan?
Ah, prostate cancer—the only condition that can make you feel like your doctor is trying to get inside your head and your pants at the same time! But fear not, dear readers; there’s a beacon of hope shining from the world of artificial intelligence (AI) and multiparametric magnetic resonance imaging (mpMRI). Recently, a study suggested that AI could give us the lowdown on tumor volume and metastasis in localized prostate cancer patients. Think of it as your prostate’s own personal assistant—except this one doesn’t complain about your coffee order.
In a study published in the esteemed Radiology journal (because what else would a stubbornly specialized journal be called?), researchers created a fancy AI tumor segmentation algorithm. Its mission? To differentiate between Prostate Imaging Reporting and Data System (PI-RADS) 3-5 lesions. You know, for that lovely afternoon when you want to kick back and see how tumors are being ranked these days.
The study took a closer look at 732 patients treated either with radical prostatectomy (RP) or radiotherapy (RT). What they found was nothing short of surprising: VAI outperformed the National Comprehensive Cancer Network (NCCN) risk classification in predicting metastasis. Who would’ve thought that an algorithm could outperform seasoned oncologists? But it seems like VAI is the new kid on the block—cool, calculating, and entirely devoid of any awkward waiting-room small talk.
Here Come the Numbers!
In the RT group, VAI had an 84% area under the curve (AUC) for predicting seven-year metastases, while the NCCN risk classification limped along at a meager 74%. As for the RP cohort, VAI boasted a cheeky 89% AUC compared to the NCCN’s 79% in predicting metastases within five years.
Lead author Dr. David D. Yang and his team noted that while the VAI model had its moments—detecting PI-RADS 5 lesions like a pro—it also missed some that made you wonder if it had a bit too much wine at dinner. It’s like how you keep losing the remote but can always find your kid’s spare Lego piece in the dark—AI might need a little refining, clearly!
Three Key Takeaways to Ponder While Avoiding Awkward Prostate Exams
- AI-assisted tumor volume measurement shows predictive advantage. The AI segmentation model (VAI) is proving to be more reliable and accurate than traditional methods. What’s next? AI giving relationship advice?
- Consistent and reproducible measurement. The study highlights VAI as a more dependable measurement for assessing intraprostatic tumor burden, even if it occasionally gets lost in the weeds like your uncle at a family wedding.
- Potential to influence treatment decisions. If you’re a high-risk patient, VAI might just nudge physicians towards recommending radiotherapy over surgery. Just like when your mate suggests a curry instead of a salad during dinner, but this time, it could save your life.
Furthermore, the authors suggest that using VAI might also change management strategies for those with unfavorable-risk disease. The algorithm could help identify patients for whom upfront radiotherapy is a smarter move, rather than waiting for things to go south after surgery.
Now, let’s not kid ourselves. It’s not all roses and sunshine. The study has its limitations—after all, it was a single-center retrospective analysis. Plus, they cautioned that the algorithm’s magic might not work with different MRI systems or image acquisition settings. It’s a bit like trying to use an English plug in a European socket; it’s just not meant to be!
So what’s the takeaway from this AI adventure in prostate cancer? Well, let’s just say that while the robot revolution is upon us, and we should probably take it seriously, it seems like VAI is proving it might just be one of the good ones. Like that friend who remembers your birthday and always brings cake, rather than just sweeping it under the rug like your last embarrassing moment!
This combination of humor, sharp commentary, and engaging narrative captures the essence of the article while making it accessible and entertaining for readers.