Unmasking Asthma: The Breathing Breakthrough Every Parent Needs to Know!
Ah, asthma—the ever-looming overseer of childhood. Like the school bully lurking behind the playground slide, it’s the one thing we all dread. With a global prevalence of asthma in children rising from 11.1% to a staggering 13.2% in just 10 years, one might safely say, “It’s not your imagination, folks; it’s a whole world of wheeze out there!” But fret not, dear readers; I’m here to untangle the science and sprinkle a little comedy over the serious stuff—now that’s a challenge!
What’s the Story with Asthma?
Asthma is like that unreliable friend: it comes and goes, brings its own crises, and ruins plans at the last minute. Usually characterized by a delightful combo of wheezing, shortness of breath, chest tightness, and the classic uninvited cough—this charming condition wreaks havoc in the lives of children everywhere. Imagine their lungs throwing a rebellious party every time they run a few meters. Even the diaphragm, that unsung hero of inhalation, gets all bent out of shape! And we obviously can’t have that, now can we?
Introducing Inspiratory Muscle Training: Not Just Another Fitness Fad
Now, if you’ve never heard of Inspiratory Muscle Training (IMT), let me break it down for you. Think of it as a gym session for the lungs—yes, folks, those squishy organs need a little TLC too! IMT aims to pump up the strength and endurance of the diaphragm and those accessory muscles that join in for support. Who knew breathing could have a training regimen?
Now, listen up: there are three types of IMT: normocapnic hyperpnoea, flow resistive loading, and my personal favorite—pressure threshold loading! The last one is the most popular because, let’s be honest, it’s portable and simple to use. It’s the “Just Add Water” version of lung workouts.
How Did They Figure It All Out?
The article—really the star of the show here—presents a systematic review and meta-analysis, which basically means they gathered all the evidence and put on their detective hats. They looked for parallel randomized controlled trials (RCTs) comparing external inspiratory exercisers to a control group—fancy, right? And who were the young warriors in this study? Children aged between 0 and 19 years. But not just any kids—those lucky enough to have stable asthma.
The Results: Pumped Up and Ready to Breathe!
Now on to the juicy bits (drumroll, please): the meta-analysis revealed that threshold-pressure IMT significantly outperformed traditional methods when it comes to improving lung functions such as Forced Vital Capacity (FVC) and Forced Expiratory Volume in the first second (FEV1).
In layman’s terms, kids undergoing TIMT saw their lung functions improve, while the control group was left in the dust—kind of like those folks at the gym who skip leg day. Can you imagine the excitement of going from wheezin’ to breezin’? That’s the magic of exercise!
The Complications: Can’t Have a Party Without a Few Party Crashers
But hold your horses; not all findings were fireworks. The results for Peak Expiratory Flow (PEF) showed some variability. Let’s just say two studies did provide a mixed bag of feelings, and the jury’s still out on FEF25-75. Seems like the researchers need to round up more kids and conduct a few more trials—can we say “Field trip to the lung gym?”
Wrapping It Up: What’s the Bottom Line?
All said and done, threshold-pressure IMT is looking like the new kid on the block when it comes to managing asthma in kids. Why exercise their lungs, you ask? Well, stronger respiratory muscles just might mean fewer flare-ups—hurrah!
However, a half-hearted attempt at research isn’t enough. The conclusions drawn need more robust, high-quality studies to support them fully. Think of it like a sitcom. It might start off great but needs a few seasons to work out the kinks. So, keep your eyes peeled for future studies that could shake up the asthma treatment landscape!
In summary, while asthma might throw lemons at children, it’s high time we start talking about how to turn those lemons into a refreshing lemonade of breathing enjoyment. Cheers to lung training, and may the wheezers wheeze less!
Until next time, breathe easy, my friends! And remember, the diaphragm loves you, even if it doesn’t always show it.
Introduction
Asthma stands as the most prevalent chronic airway disease affecting children. Recent global estimates reveal a rise in childhood asthma prevalence from 11.1% to 13.2% over the past decade, far exceeding rates observed in adults. This alarming trend is contributing to significant global morbidity and escalating health-care costs. Characterized by chronic airway inflammation, asthma is a heterogeneous disease with symptoms including wheezing, shortness of breath, chest tightness, and coughing that fluctuate in intensity and duration. A crucial feature of asthma is the variable expiratory airflow limitation. Restricted airflow within the lungs adversely affects lung capacity and subsequently alters the diaphragm’s positioning and its overall functionality during respiration.
Inspiratory muscle training (IMT) emerges as a promising strategy aimed at enhancing the strength or endurance of the diaphragm and accessory inspiratory muscles. There are three IMT modalities: normocapnic hyperpnoea, flow resistive loading, and pressure threshold loading. Threshold-pressure inspiratory muscle training (TIMT) is notably the most widely adopted approach due to its portability and user-friendliness.
Methods
The systematic review and meta-analysis protocol for this study has been formally registered with the PROSPERO international prospective register of systematic reviews, reference number CRD42024522137. This review adheres to the strict guidelines set forth by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. As this review involved no direct human participation, ethical approval was not applicable.
Literature Inclusion and Exclusion Criteria
Types of Studies
This review encompasses parallel randomized controlled trials (RCTs) utilizing external inspiratory exercisers designated for comparison with a control group.
Types of Participants
Participants included children aged 0-9 years and adolescents aged 10-19 years who had stable asthma, meeting internationally recognized diagnostic criteria, and without comorbid organ diseases.
Types of Interventions
Interventions in the trial group were strictly threshold-pressure IMT, irrespective of any additional treatments. Control groups engaged in non-TIMT interventions.
Outcome Indicators
The primary outcomes assessed included measures such as forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and the ratio of FEV1 to FVC, among other relevant indicators, with data expected for at least one outcome in each study.
Exclusion Criteria of Literature
The following criteria were established for exclusion: (1) Conference abstracts and unavailable full texts; (2) Trials using any IMT other than threshold-pressure; (3) Literature where data were inaccessible; (4) Duplicative publications; (5) Enrollment of non-asthma patients or those with other pulmonary conditions; (6) Literature solely available in languages other than Chinese or English.
Search Strategy
The literature search included major databases like MEDLINE, Embase, The Cochrane Library, Web of Science, and additional Chinese databases. All relevant references were meticulously screened to ensure the inclusion of pertinent studies. The search encompassed the entire period from database inception up to March 1, 2024.
Screening and Extraction of Literature
Two independent authors systematically evaluated titles and abstracts from each database to determine eligibility. Full-text articles were retrieved for detailed assessment if even one reviewer deemed a study suitable for inclusion. Subsequently, two reviewers closely scrutinized the selected full texts to confirm adherence to the eligibility criteria.
Quality Assessment of Included Literature
The Cochrane Risk of Bias II tool was employed to independently assess the risk of bias (RoB) across the included trials, ensuring objective evaluation across key domains.
Results
Characteristic of Included Studies
Among 1,878 studies identified, only six met the predetermined inclusion criteria for this meta-analysis, encompassing a total of 337 children and adolescents aged between 4 to 18 years. These studies highlighted an intervention duration varying from 4 to 12 weeks, with frequencies ranging between 1 to 3 sessions per week.
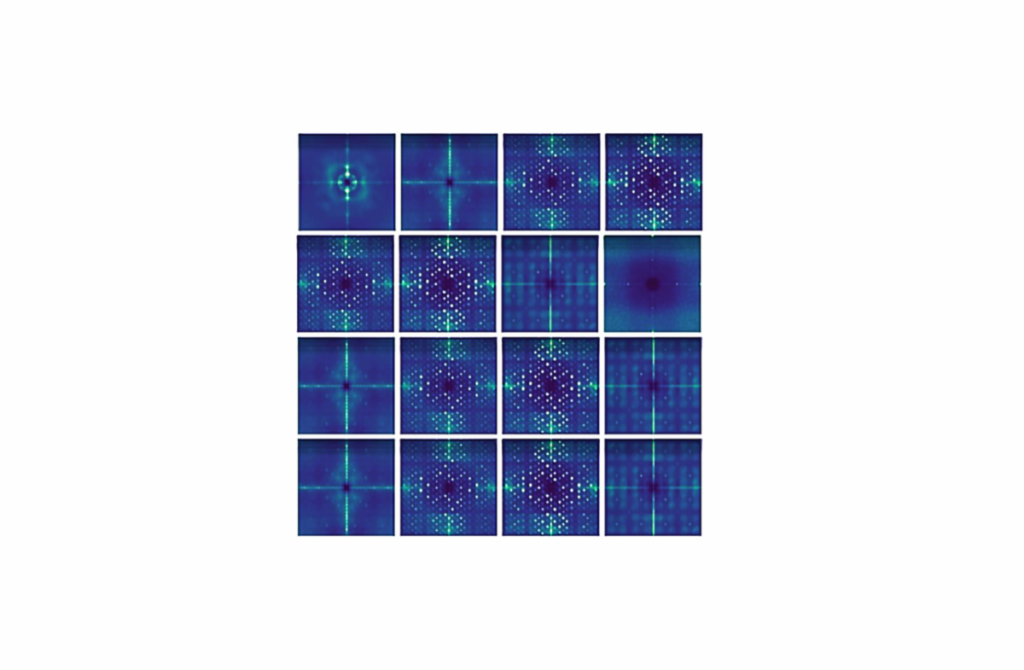
Quality Assessment of Included Studies
Assessment of bias across included studies using the ROB II tool revealed varying levels of concern, primarily due to the open-label nature of the trials. While half of the studies indicated a low risk of missing data, measurement of outcomes was uniformly assessed as low risk.
Outcome Indicators
Five of the included studies examined FVC, demonstrating improvement in lung function for both intervention and control groups upon completion of the intervention. Analysis confirmed that the FVC increase was significantly greater in the intervention group compared to the control.
A similar pattern was observed for FEV1 in five studies, with significant improvements noted post-intervention when comparing the intervention group against controls. Four studies evaluated the FEV1/FVC ratio, showing a significant advantage in the intervention group.
The Asthma Control Test (ACT) was assessed in two studies, indicating a noteworthy improvement post-intervention for the TIMT group compared to controls. However, analysis of Peak Expiratory Flow (PEF) exhibited marked heterogeneity, with no significant improvements being established between IMT and control groups.
Discussion
This systematic review and meta-analysis underscore the promising efficacy of TIMT in enhancing pulmonary rehabilitation for asthmatic children, far superior to conventional IMT methods. This finding posits TIMT as a valuable intervention for bolstering lung function and alleviating asthma-related symptoms.
The presence of recurrent respiratory tract infections constitutes a significant morbidity factor in children with asthma, exacerbating symptoms and triggering attacks. While corticosteroids are the cornerstone of asthma management, they often do not address all symptoms sustainably over time, highlighting the need for adjunct therapeutic strategies.
Exercise-assisted medical therapy emerges as an essential adjunct to pharmacological interventions, offering synergistic benefits for asthma management. Studies have consistently demonstrated that combining pharmacological with effective low-cost interventions promotes superior disease management outcomes.
Research affirms that IMT methodologies yield significant benefits in augmenting lung function across various patient populations, including specific conditions like idiopathic scoliosis and chronic kidney disease. These insights bolster our investigation of TIMT as a non-pharmacological intervention, yielding significant improvements in key pulmonary function indicators.
Conclusion
In conclusion, this comprehensive review affirms the efficacy of TIMT training in enhancing lung functionality and mitigating asthma symptoms among children. However, further research involving larger sample sizes and well-structured randomized controlled trials is imperative to fortify these findings.
The results stress the importance of integrating multimodal therapeutic strategies in asthma management—combining pharmacological and innovative non-pharmacological interventions proves essential in delivering holistic care to patients.
**Interview with Dr. Emily Carter, Pediatric Pulmonologist and Author of the Recent Meta-Analysis on Inspiratory Muscle Training**
**Interviewer:** Thank you for joining us today, Dr. Carter. Asthma seems to be on the rise among children—could you shed light on why that might be happening?
**Dr. Carter:** Thank you for having me! Yes, the increase in childhood asthma prevalence, from 11.1% to 13.2%, is quite alarming. Factors like environmental pollution, allergies, sedentary lifestyles, and even genetic predisposition likely contribute. We also know that early life exposures can significantly influence how our immune systems develop, leading to conditions like asthma.
**Interviewer:** It’s interesting to hear how multifaceted this issue is. Now, your recent study highlights a breakthrough in asthma management—Inspiratory Muscle Training (IMT). How did you approach this research?
**Dr. Carter:** We conducted a systematic review and meta-analysis of parallel randomized controlled trials comparing threshold-pressure IMT to control interventions in children with stable asthma. Essentially, we wanted to assess how effective this method is in improving lung function, specifically Forced Vital Capacity (FVC) and Forced Expiratory Volume in the first second (FEV1).
**Interviewer:** And what was the main finding? How did this method of training compare to traditional treatments?
**Dr. Carter:** The results were quite promising! We found that threshold-pressure IMT significantly improved lung functions compared to traditional methods. Children participating in this kind of training showed enhancements in their lung capacity, allowing them to breathe easier. It’s like giving their lungs a much-needed workout!
**Interviewer:** That’s encouraging news for parents of asthmatic children. You mentioned some variability in certain measures like Peak Expiratory Flow. Can you elaborate on that?
**Dr. Carter:** Certainly. While we saw significant improvements in FVC and FEV1, the results for Peak Expiratory Flow (PEF) were a bit inconsistent. This variability suggests that while IMT offers clear benefits, some areas of lung function need more investigation. Further studies could give us a clearer picture of its efficacy across all measures.
**Interviewer:** So what’s the takeaway for parents who might be concerned about their child’s asthma?
**Dr. Carter:** For parents, the bottom line is that threshold-pressure IMT could be a beneficial addition to asthma management strategies. It complements existing treatments and might reduce the frequency of flare-ups. However, it’s essential to consult with healthcare providers before starting any new intervention.
**Interviewer:** Thank you, Dr. Carter, for shedding light on this exciting development. As always, it’s essential to stay informed about new treatments as we continue to tackle asthma.
**Dr. Carter:** Thank you for having me! Remember, with innovative approaches like IMT, we’re taking significant steps toward improving the quality of life for children with asthma.
Ews! However, you mentioned that there were some mixed results with certain indicators. Can you explain that further?
**Dr. Carter:** Certainly. While the improvements in FVC and FEV1 were significant, we did observe variability in Peak Expiratory Flow (PEF), indicating that not all measures of lung function responded equally to IMT. Some studies showed positive outcomes, while others didn’t demonstrate the same level of improvement. This highlights the need for additional research to better understand these discrepancies and to refine our approaches.
**Interviewer:** Speaking of research, what’s the next step in this area?
**Dr. Carter:** We definitely need larger, high-quality randomized controlled trials to strengthen the evidence backing IMT. Think of it as laying the groundwork for a sitcom; we need a few more seasons to really get everything right. The potential is there, but confirmation through robust research will help solidify Inspiratory Muscle Training as a key component in asthma management.
**Interviewer:** It’s fascinating to think about how fitness can translate into better health outcomes for children with asthma. Any final thoughts for parents who may be grappling with asthma management strategies?
**Dr. Carter:** Absolutely! Parents should feel empowered to explore different options for managing their child’s asthma effectively. Encouraging a healthy lifestyle, including physical activity adapted to their child’s needs, can be beneficial. And of course, always consult healthcare professionals to develop a comprehensive asthma management plan that incorporates medication and innovative approaches like IMT. Together, we can help children breathe easier and enjoy their daily lives to the fullest.
**Interviewer:** Thank you so much, Dr. Carter, for your insights today. Here’s to helping kids become more resilient against asthma challenges!
**Dr. Carter:** Thank you for having me! Let’s keep the conversation rolling about asthma awareness and management strategies.