MPox or monkeypox has once again triggered alerts for health services, as the World Health Organization (WHO) has declared a public health emergency of international importance on August 14, 2024 due to a new outbreak caused by a subvariant.
With this announcement, the WHO hopes that there will be a coordinated international response to keep the disease under control.
The aim is to strengthen prevention and diagnostic methods, as well as to speed up research into the infection and thus curb its transmission.
Following this alert by the WHO, the disease monkeypox is once again generating concern and questions.
How serious has the disease become due to this strain? How did mpox become a health emergency again? How is it transmitted and what are its symptoms? Are there vaccines to prevent it? What have health authorities in Guatemala said?
The answers to these questions have been provided through WHO alerts, reports, and communications. Here is a summary of the latest developments.
How did the new mpox outbreak declared as an emergency arise?
The African region began reporting cases of a variant in September 2023, which had been circulating in its eastern region.
Since then, by early August 2024, the outbreak has spread to 15 African countries, including four that had not previously been affected by the disease, and which began reporting cases from mid-July 2024.
Given its spread in that region, a global health alert was activated.
By Thursday, August 15, Swedish health authorities confirmed one case, the first confirmed in Europe, and on Friday, August 16, a patient was also confirmed in Pakistan.
What is the new variant of monkeypox and how did it arise?
The monkeypox virus, which belongs to the genus Orthopoxvirus, includes the virus that causes smallpox.
MPox, or monkeypox, was first detected in Africa in 1970. It was not until a decade ago that it was detected in the Republic of the Congo, and cases have continued to increase since then.
There are two genetically distinct strains of the mpox virus: Congo Basin strainin central Africa, called “clade 1”and the West African strainunder the nomenclature “clade 2”.
Human infections, it is the clade 1 subvariant—the strain in the Congo Basin—that is behind this new outbreak in 2024.
The previous outbreak affected homosexual populations more, but the new data indicate that the new strain is being transmitted more widely, probably initially through sexual contact and then to a close circle.
Local health services in Africa detected from the first outbreak that mine workers were seeking the sexual market, which led to the disease spreading.
However, as is the nature of a virus, by adapting to its host, it appears to have evolved and the clade 1 subvariant is spreading to a greater number of people.
The rapid spread of clade 1b in the Democratic Republic of the Congo and its detection in neighbouring countries is “particularly worrying”, said WHO director Tedros Adhanom on 14 August in his speech at the start of a meeting with the organisation’s Emergency Committee.
“We are not dealing with an outbreak of a single clade; we are dealing with several outbreaks of different clades in different countries with different modes of transmission and different levels of risk,” he said.
Read also: Stress-induced illnesses: How to prevent and alleviate them

How is it transmitted and what are its symptoms?
Historically, cases have occurred through contact with infected wild animals, hunting, skinning or cooking them, or consuming infected meat.
Once transmitted to humans, The disease has evolved and in addition to being transmitted sexually, it also spreads through contact with bodily fluids. from an infected person, by touching or kissing them, or simply by having contact with contaminated materials, such as clothing or bedding, as well as needles used by those who have the virus.
Besides, Pregnant women can transmit the virus to the fetus.
Monkeypox is characterized by a rash or skin lesions that are usually concentrated on the face, palms of the hands, and soles of the feet, according to the Pan American Health Organization (PAHO).
Signs and symptoms
Signs and symptoms usually begin about a week after exposure, but may occur within 1 to 21 days.
Symptoms usually last 2 to 4 weeks, or longer in people with a weak immune system.
Common symptoms, according to the WHO:
- skin rash
- fever
- sore throat
- headache
- muscle pains
- backache
- lack of energy
- swollen lymph nodes.
Although the first symptom is usually a rash, other different symptoms may appear earlier.
The eruption begins as a spot that turns into a fluid-filled blister and may be itch or painful. According to the WHO, as the rash heals, the lesions dry out and become covered with scabs that eventually fall off.

Skin lesions may be just a few or hundreds, says the WHO.
These lesions can appear anywhere on the body, such as:
- palms of the hands and soles of the feet
- face, mouth and throat
- English and genitals
- again
Some symptoms that occur are painful swelling of the rectum or pain and difficulty urinating.
An important point that the WHO emphasizes is that Patients are contagious until all lesions have healed and the skin has renewed.
The Organization says that the most vulnerable groups include children, pregnant women and immunosuppressed people, as they are at risk of suffering complications.
The risk of severe illness and death increases in patients with a weakened immune systemwhether due to medication or a previous or chronic condition.
Severe illness has been seen more frequently in patients with HIV that is not well controlled.
Why is vaccination not widespread?
Unlike other diseases such as Covid-19, the health system has a vaccine developed against monkeypox that can help prevent infection.
This vaccine should be administered within 4 days of contact with someone who has monkeypox, and according to the WHO, it can be administered even up to 14 days later if there are still no symptoms.
The WHO believes that it is not necessary to call for mass immunization at this time because existing vaccines are being prioritized, especially for health personnel at risk of exposure or people who have had contact with infected patients.
The main reason is that there are not so many vaccines produced worldwide.
Therapy has thus far been more focused on treating symptoms and preventing complications.
Several antivirals have been used in the treatment of monkeypox, such as tecovirimat, which was developed to treat smallpox.
What have health authorities in Guatemala said?
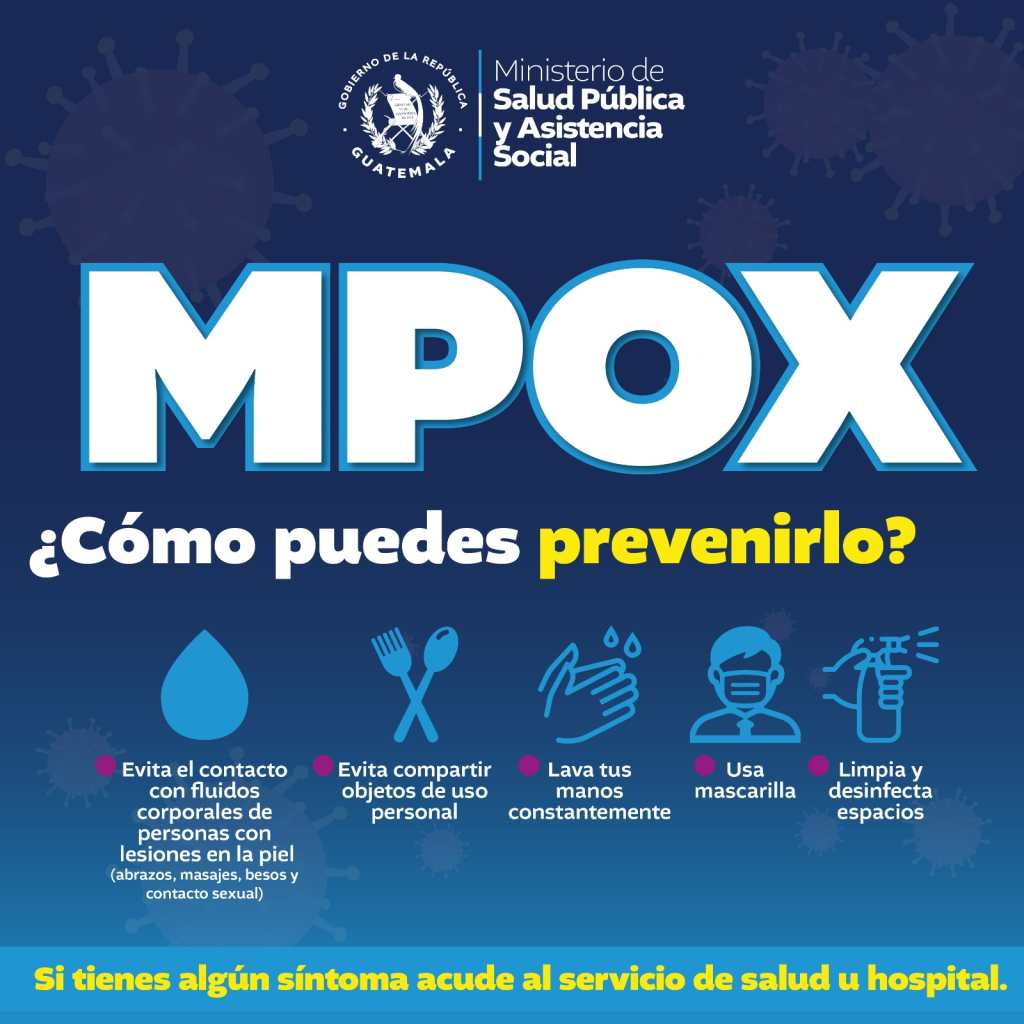
Guatemala has no confirmed cases so far, but remains on alert to protect the population. The Ministry of Health and Social Assistance (Mspas) asked people to avoid alarm and stay informed through official media.
To prevent infection and alleviate symptoms, patients should stay home, wash their hands frequently, wear a mask, and cover lesions when around others.
- Stay at home, preferably in your own room.
- Wash your hands frequently with soap and water or hand sanitizer, especially before and after touching the lesions.
- Wear a mask and cover the lesions when around others until the rash has healed.
- Keep skin dry and uncovered, except when in the same room with other people.
- Avoid touching objects in shared spaces and disinfect them regularly.
- Rinse with salt water if there are lesions in the mouth.
- Take sitz baths or warm baths with baking soda or Epsom salt to relieve body injuries.
- Take over-the-counter pain medications, such as paracetamol (acetaminophen) or ibuprofen.
Read also: Immune system: Four habits that strengthen it
#monkeypox #transmitted #clade #variant #situation #Guatemala
