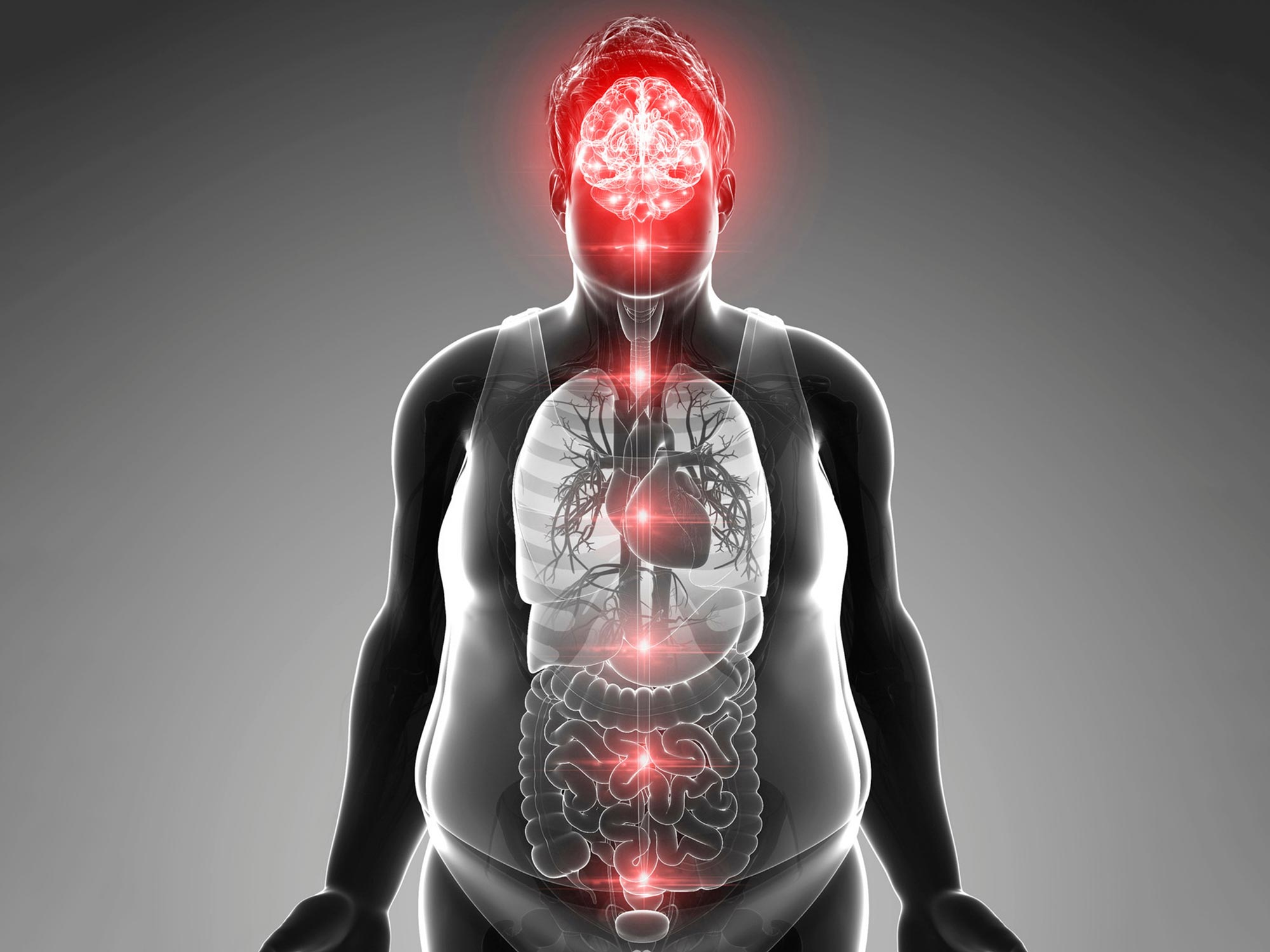
Middle-Age Obesity Linked to Brain Structure Changes, Study Finds
A recent study conducted by researchers at Nagoya University and their colleagues in Japan has shed light on the connection between middle-age obesity and age-related alterations in brain structure. The study, published in the journal Cell Metabolism, suggests that obesity in middle age may be caused by the shortening of specific brain structures that regulate metabolism, emphasizing the importance of dietary management in prevention.
The research team focused on a protein called melanocortin-4 receptor (MC4R) which plays a crucial role in detecting overnutrition and regulating metabolism and appetite to prevent obesity. By examining MC4Rs in rats, they discovered that these receptors are concentrated in primary cilia, antenna-like structures that extend from certain groups of hypothalamic neurons. As rats aged, the primary cilia became shorter, resulting in a decrease in MC4Rs and subsequent weight gain.
“We believe that a similar mechanism exists in humans as well,” said Professor Kazuhiro Nakamura of Nagoya University Graduate School of Medicine. “We hope our findings will lead to a fundamental treatment for obesity.”
The mechanism behind middle-age weight gain has long been a topic of interest. While previous studies have suggested a decline in overall metabolism due to aging, the specific mechanism was unclear. This recent study provides valuable insights into the processes at play.
The research team, in collaboration with other institutions, conducted further investigations by analyzing MC4R cilia under different dietary conditions. They found that MC4R cilia gradually shortened with age in rats on a normal diet and at a faster pace in rats on a high-fat diet. Interestingly, rats subjected to a restricted diet displayed a slower pace of MC4R cilia shortening. Furthermore, the team observed that MC4R cilia that had disappeared with age were regenerated in rats raised under two months of dietary restriction.
One notable discovery was the phenomenon of leptin resistance, which was observed in rats with artificially shortened MC4R cilia. Leptin, a hormone that helps reduce food intake, was administered to these rats but failed to exert its anti-obesity effects. Leptin resistance is often observed in obese human patients, but its cause has remained unknown until now.
The implications of this study extend beyond the understanding of middle-age obesity. It opens up possibilities for developing treatments and interventions that target the age-related shortening of MC4R cilia. Furthermore, the focus on dietary management as a preventive measure emphasizes the importance of maintaining healthy eating habits throughout life.
Looking ahead, this research raises important questions regarding the future of obesity prevention and treatment. As the global obesity epidemic continues to rise, it is crucial to explore innovative approaches that address the underlying causes of weight gain. By understanding the mechanisms behind middle-age obesity, researchers can develop targeted interventions, potentially revolutionizing the way obesity is managed.
In conclusion, this study highlights the intricate connections between brain structure, metabolism regulation, and obesity. It provides valuable insights into the factors contributing to middle-age weight gain and emphasizes the importance of dietary management in prevention. As the field of obesity research advances, it is essential to continue investigating these connections and develop strategies to combat this growing health issue.