2023-04-21 00:01:32
We are on the brink of a global crisis of an infectious disease from which no country is immune and no country can rest easy.
In the World Health Report published by the World Health Organization in 1996, the above passage warned the world that at least 17 million people die from infectious diseases every year, and the control of infectious diseases will become increasingly difficult. Around this time, Ebola filovirus and H1N1 bird flu with a fatality rate of 50% appeared in the world, as well as Nipah paramyxovirus with a fatality rate of 20%.
At that time, the coronavirus was not noticed and considered a threat to human beings.
Coronavirus’s first “epidemic” SARS outbreak
In November 2002, a similar case of pneumonia was reported in Guangdong Province, China. The patient had fever, dry cough, and difficulty breathing due to pneumonia. The Chinese authorities dispatched an investigation team in January, and held a press conference in Guangdong Province on February 10, stating that 305 people in Guangdong had suffered from “atypical pneumonia” and 5 died, but the epidemic had been effectively controlled, emphasizing that compared with Guangzhou, thousands of With a population of 10,000, atypical pneumonia only occurred locally.

At this time, the World Health Organization (WHO) and the world are still unaware that the news of China’s blockade of SARS has spread, and this emerging disease is evolving into a major epidemic that impacts the modern medical system. Until March, confirmed cases were reported in other countries, and the WHO became alert. Jiang Yanyong, a retired Chinese military doctor known as the “SARS whistleblower”, also warned the world.
China hides the epidemic and runs away
“As a doctor who cares regarding people’s lives and health, I have the responsibility to assist international and local efforts to prevent the spread of SARS.” On April 8, 2003, Jiang Yanyong, who lives in Beijing, China, wrote a letter to the international media to expose the SARS epidemic in China and stated Make public the Chinese authorities’ cover-up of the epidemic.

The United States “Time Magazine” was the first to disclose Jiang Yanyong’s letter and pointed out that as of April 8, doctors at the 309th Hospital of the People’s Liberation Army in Beijing told Jiang Yanyong that they had admitted 60 SARS patients and seven of them died; but on April 3, the Chinese Ministry of Health Minister Zhang Wenkang announced to the media that only 12 SARS cases were found in the Chinese capital, of which 3 died.
Jiang Yanyongxin stated that the medical staff of the PLA Hospital in Beijing had been informed of the danger of atypical pneumonia as early as the beginning of the National People’s Congress in early March, and were asked not to disclose it.
Jiang Yanyong’s warning letter forced the Chinese government to disclose the situation of SARS prevention and control work, and fired Zhang Wenkang, the party secretary of the Ministry of Health at the time, and Meng Xuenong, deputy secretary of the Beijing Municipal Party Committee, for improper handling of the epidemic. However, the SARS epidemic that originated in Guangdong had already spread. It spread to North China in early March and spread to 26 provinces and cities in mid-to-late April.
The chain of transmission of the virus also crossed out of China in late February. According to the WHO’s subsequent investigation, Liu Jianlun, a 64-year-old professor of medicine at Sun Yat-sen University in Guangzhou, was the first recorded super-spreader of the SARS virus.

Liu Jianlun arrived in Hong Kong on February 21 and died of illness in Hong Kong on the 23rd. The hospital also failed to detect it in time, and nosocomial infections broke out. die. And Liu Jianlun stayed in a hotel in Hong Kong before his death, which also caused 13 passengers to be infected, and spread the virus to Hong Kong, Canada, Vietnam, Germany and Singapore.

The World Health Organization (WHO) issued a global emergency travel warning on March 15, stating that it had received more than 150 suspected cases of Severe Acute Respiratory Syndrome (Severe Acute Respiratory Syndrome) of unknown etiology in the past week, including those from Canada. , China, Hong Kong, Indonesia, Philippines, Singapore, Thailand and Vietnam. This is also the first time the WHO named the disease SARS.
On April 16, 2003, the World Health Organization officially confirmed that SARS coronavirus (SARS-CoV) was the pathogen of SARS. At that time, the virus had already quietly arrived in Taiwan.
Nosocomial infection broke out in Taiwan-occupied Heping Hospital and the hospital was closed
The investigation published by the Epidemiological Administration in the Special Issue on SARS Epidemic Prevention pointed out that there have been imported cases in Taiwan since March. At that time, the epidemic prevention and control were said to be smooth. Until March 29, a Ms. Cao claimed to be suspected of being infected by a coughing passenger on the train. , the symptoms did not improve following treatment in three clinics; on April 9th, he went to Heping Hospital to take X-rays and was judged to be suspected of SARS; but the hospital did not disinfect the isolation gowns in the X-ray room that day, which caused the outsourced laundryman surnamed Liu Infected while washing the isolation gown.
The laundry worker developed a fever and diarrhea on April 12, and was hospitalized on April 16. Cluster infections broke out in the hospital. On April 24, the Taipei City Government ordered the Heping Hospital to be closed, hoping to control the epidemic. 346 people were diagnosed and 73 people died, including 7 medical staff who died in the line of duty.
In the end, the SARS virus spread to 29 countries, causing 8,096 infections and 774 deaths. Until July 5, 2003, the World Health Organization announced that the last chain of human-to-human transmission of SARS had been broken, the epidemic was over, and the virus disappeared for 20 years.
However, He Meixiang, an epidemiologist at the Academia Sinica, said that SARS is an ancient virus in animals. The epidemic on humans has ended, but it still continues to survive in the original host—bats.
Lessons from the coronavirus: a global pandemic crisis
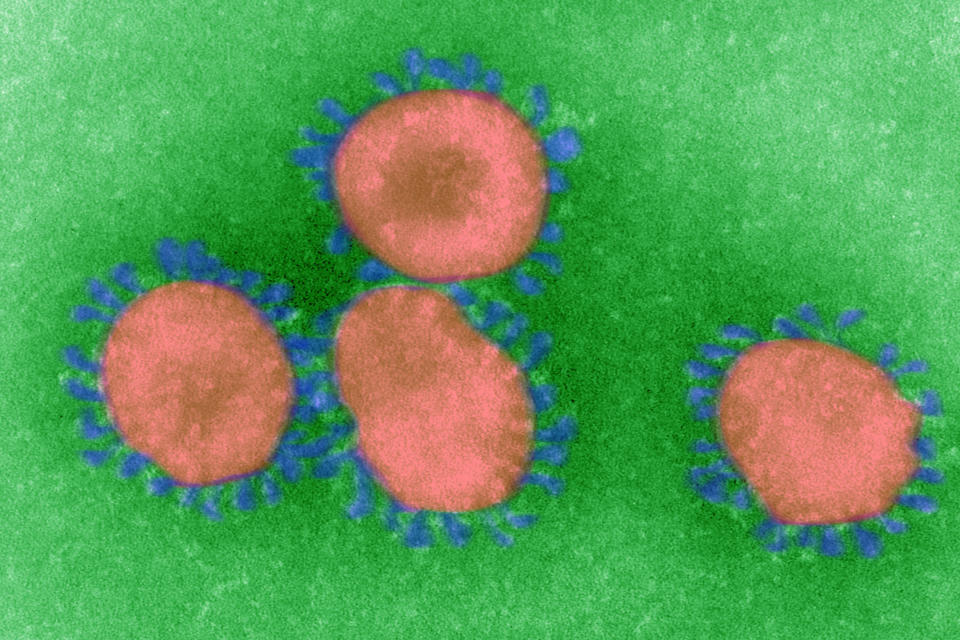
Since 1960, British virologist Dr. Almeida (June Almeida) first discovered coronavirus on a British student’s specimen through a microscope, and published the research results in 1965 to name it. It has been nearly 50 years since For 20 years, humans have not considered this family of viruses with crowned protrusions on the cell membrane to be a threat.
Embed from Getty Images
So far, a total of 7 coronaviruses infecting humans have been identified in the world: HCoV-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1, SARS-CoV, MERS-CoV and SARS-CoV-2. Only causes common cold symptoms. However, since SARS, coronaviruses have brought deadly emerging diseases to humans every less than 10 years, including Middle East Respiratory Syndrome Coronavirus Infection (MERS) and COVID-19.

The MERS-CoV virus broke out in 2012 with the Middle East Respiratory Syndrome Coronavirus infection, and the fatality rate was as high as 36%. There were still outbreaks during the FIFA World Cup in Qatar last year. Although the number of cases exported from the Middle East is increasing around the world, except for the suspected local infection in South Korea in 2015, there are few subsequent cases of infection outside the Middle East.
The SARS-CoV-2 virus has caused the COVID-19 epidemic since 2019. According to the World Health Organization, as of April 2023, there have been more than 700 million confirmed cases and more than 6 million deaths. The virus is still spreading around the world.
Vaccines cannot clear the virus, what is the next step for humans?
Although why did SARS suddenly disappear? Will MERS spread beyond the Middle East once more? There are still puzzles to be solved, but more than 13 billion doses of vaccines have been administered around the world to eradicate COVID-19, the greatest plague in human history, according to the World Health Organization. However, Chen Xiuxi, a professor of public health at National Taiwan University, said that from the experience of COVID-19, the vaccine has limited effect on preventing and blocking the coronavirus. warning line.
He Meixiang also believes that following the outbreak of the epidemic, Pfizer, which was the first to develop a COVID-19 vaccine within a year, was hailed as achieving an impossible mission like “landing on the moon”, but even if new technologies allow humans to develop a new vaccine Vaccines can be shortened to 100 days at the earliest. When facing emerging infectious diseases next time, “We must think regarding whether we can withstand the initial 100-day spread of the epidemic?”
At present, there is no conclusion regarding the intermediate host through which the SARS-CoV-2 virus is transmitted from bats to humans. Studies collected by the U.S. Department of Health Services show that following genetic analysis, SARS-CoV-2 may also have originated from pangolins, and that SARS-CoV-2 was sampled at a high rate in Malayan pangolins. The study also pointed out that pangolins are the mammals with the most illegal wildlife smuggling. If the wildlife trade cannot be effectively controlled, pangolin coronaviruses may pose a threat to public health.
Recalling that the outbreaks from SARS to COVID-19 all originated in China and were related to contact with wild animals. He Meixiang pointed out that the three coronaviruses are all cross-species transmission, which shows that as the habitats of humans and animals overlap more and more, it will give more harm to humans. There are new opportunities for viruses to cause diseases to humans. Even if the live animal market for selling wild game continues to exist, new epidemics will inevitably recur; Risk of virus exposure.
Chen Xiuxi also reminded that the long-term new crown phenomenon also provides a new evidence that the coronavirus can survive for a long time in humans with poor immunity. This phenomenon may promote virus mutation; in addition to monitoring the relationship between humans and ecological animals in the future, it is also necessary to monitor the coronavirus In the development of the human body, a two-pronged approach is taken to prevent the advent of new epidemics.
More PTV news reports
Taiwan and Japan cooperate to send “like viruses” to the sky, hoping to improve the effectiveness of vaccines
1682048216
#years #SARS #pandemic #era #SARS #COVID19 #teach



