As its name suggests, a colectomy is a surgical procedure that consists of remove part or all of the colon. Depending on the case, a distinction is made between right colectomy, transverse colectomy, left colectomy and sigmoidectomy (removal of the sigmoid colon). How does this type of intervention take place? When is it recommended? What precautions to take? Responses from Dr Aurelien Dupresurgeon specializing in digestive oncology at the Léon Bérard cancer center (Lyon).
Definition: what is a colectomy?
Colectomy is THE standard treatment for colon cancer, says Dr. Dupré straight away. It most often consists of remove a piece of colon before restoring the intestinal circuit by anastomosis. “In practice, in the context of colon cancer, for example, the cancerous cells are removed with a safety margin, then connect the two parts of the colon“, he explains.
As a reminder, the role of the colon is to absorb water from our stools to make them more compact. Together with the rectum, it constitutes the large intestine, the last part of our digestive tract. Unlike the small intestine (the small intestine), it plays no role in the absorption of food
Total, enlarged or partial colectomy?
Most often, colectomy requires remove a single segment of the colon : we therefore speak of a partial colectomy.
An “enlarged” colectomy may sometimes be necessary: it consists of remove several segments of the colonfor example the right and transverse segment, or the left and transverse segment.
In much rarer cases, the situation requires removal of the entire colon : we speak of total colectomy.
Right, left, transverse or sigmoidectomy colectomy?
The colon is made up of several segments. Depending on the segment affected, we therefore distinguish between different types of operations:
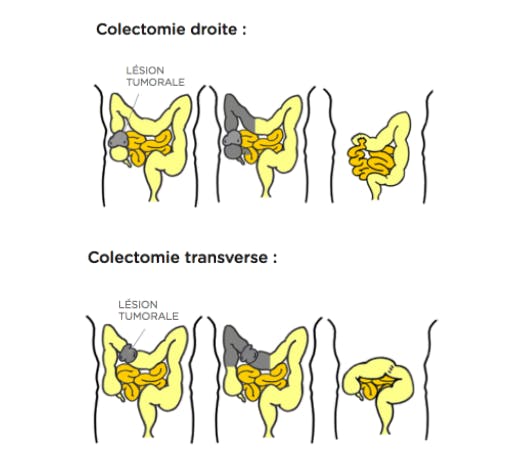
- right colectomywhich consists of removing the right part of the colon (also called ascending);
- the transverse colectomywhich consists of removing the transverse part of the colon (which connects the right colon to the left colon);
- left colectomywhich consists of removing the left part of the colon (also called descending);
- sigmoidectomywhich involves removing the sigmoid colon (which connects the left colon to the rectum).
Indications: when and why do a colostomy?
This digestive surgery can be indicated in the context of several pathologies:
- and Colon Cancer ;
- the presence of a polyp too large or likely to degenerate into cancer ;
- a diverticular sigmoiditis (an inflammation of one or more diverticula located in the sigmoid colon);
- a chronic inflammatory bowel disease (IBD), such as Crohn’s disease and ulcerative colitis.
What precautions should be taken before removing a segment of the large intestine?
Contrary to what one might think, colectomy does not require no specific preparation of the colon, assures Dr. Dupré. Forget specific diets or uncomfortable purges! However, if it makes you feel more comfortable, choose a diet low in fiber, take your precautions on the saddle and use an enema bulb before your admission.
You will be hospitalized a few hours before the intervention. However, a few precautions are necessary to promote its smooth running and success:
- stop eating at least 6 hours before the intervention;
- prefer sugary drinks (ice tea, fruit juice, etc.) and stop drinking at least 3 hours before the intervention;
- quit smoking (or at least strongly limit your consumption) some time before the operation to promote healing;
- regarding alcohol, avoid drinking for seven days before the operation. On D-Day, banish it completely.
How is a colectomy performed? How long does it last?
The colectomy generally lasts between 1h30 and 3 hours in the operating room, under general anesthesia. “It is realized par the goalioscopie : we access the inside of the abdomen through small incisions in the abdominal wall, in which we introduce a microcamera and micro-instruments”, specifies Dr. Dupré. In the event of a complication, the medical team may, however, change his mind during the procedure and practice a laparotomy more or less wide.
Anyway, the principle remains the same. The medical team begins by placing a urinary catheter and a gastric catheter at the start of the operation. Comes next la phase d’observation. In the case of colon cancer, the surgeon examines the large intestine to see the extent of the tumor. He also makes sure that the metastases have not reached other organs, such as the liver, stomach or pancreas.
It is then time to remove the affected segment, taking care to mark safety margins to limit the risk of local recurrences.
Concretely, the entire tumor is extracted and a healthy portion of tissue is also removed from both sides (regarding 5 centimeters), explains Dr. Dupré.
In case of polyp or colon cancer, the surgeon also performs lymph node dissection : it removes the vessels and ganglia close to the tumor to find out whether they contain – or not – cancerous cells.
Then comes the time to sew the ends of the remaining segments using wires (manual anastomosis) or using mechanical clamps and staples (mechanical anastomosis). Whatever the technique used, the objective is to restore the intestinal tract to ensure good digestive continuity.
Good to know: in the event of a complete colectomy, the medical team will ask a digestive stoma, in other words an artificial anus, which allows the evacuation of stool into a dedicated pocket. This device is essential for life because we do not practice either the transplant or the placement of colon prosthesis. A temporary stoma can also be placed in the event of a partial or extended colectomy.
© Center hospitalier de Luxembourg (source 2)
Colectomy by laparoscopy or laparotomy: what postoperative consequences?
The duration of postoperative hospitalization depends on several factors: the type of intervention performed, the state of health of each patient and his reaction to the anesthesia. Before signing an exit permit, the medical team ensures:
- of l’absence d’infection,
- of the absence of post-operative pain,
- and some good resumption of intestinal transit,
Any drains and urinary catheters are also removed according to the surgeon’s recommendations. Taking anticoagulant medication and wearing compression stockings are also often recommended.
“If the colectomy follows colon cancer, we often resort to at chemotherapy sessions to limit the risk of recurrence”, underlines Dr. Dupré. The sessions are generally held every two weeks, for three to six months depending on the stage of the cancer before the intervention.
Good to know: laparoscopy helps to limit post-operative pain and complications. Depending on the case, it also makes it possible to reduce the operating time, and therefore the duration of general anesthesia. Another advantage, scars following a laparoscopy are much less visible than the vertical scar traced in the middle of the abdomen in case of laparotomy.
What are the potential complications of this colon surgery?
Complications related to a colectomy remain exceptional.
During the intervention, the team may face hemorrhagic complications. In the short term, the colectomy can cause an infection, even an abscess at the level of the scar.
“But the most worrying of the complications is anastomotic fistula (a leak at the intestinal seam)”, warns Dr. Dupré. And to insist: “If the seam becomes infected and leaks, it can lead to a peritonitisa generalized infection in the abdomen, which is most often manifested by fever associated with abdominal pain and stopping of digestive transit”. This justifies close monitoring in the days following the operation. The management of this complication depends on its severity: we can bet on antibiotics and / or a new surgery to place a temporary stoma.
How are the stools following a colectomy?
In the short / medium term, transit disorders are very common: increased number of stools, diarrhoea, constipation, etc. Nothing abnormal, since part of your colon was removed: your body must adapt!
In detail, the larger the portion of the colon removed, the softer the stools. And in case of total colectomy, diarrhea can be very important during the first months. “Many patients also report a significant increase in their gases,” says Dr. Dupré. Only solutions? Patience, coupled with a suitable diet.
Rest assured, the medical team explain all the details of the procedure and the specific post-operative care to your situation!
How is recovery going? What follow-up following the intervention?
Recovery can be divided into two parts: the post-operative period and the recovery time at home. The post-operative period can last three to ten days. It allows the medical team to ensure that patients regain their normal abilities, do not suffer from abnormal pain and do not present complications. As noted above, dressings and scars are regularly monitored by nurses who also gradually remove drains and other catheters. The medical team then accompanies the resumption of food. Objective: not to rush the digestive system.
Recovery time can take several months. It allows the patient to find a less “capricious” transit. In the event of diarrhoea, transit retardants can be prescribed, alongside the monitoring of a diet low in residues. Some patients also find weight losswhich will be quickly corrected when they resume a “classic” diet.
When it comes to sports and physical exertion, doctors generally recommendavoid physical exertion for at least two months, at the risk of delaying healing. However, it is possible to resume your daily activities as soon as you return home. Regarding the return to work and driving, ask your doctor for advice.

