[팜뉴스=김응민 기자] At the 11th International Conference ICoLA 2022, held at the Conrad Hotel in Seoul from September 15 to 17 by the Korean Society of Lipid and Arteriosclerosis, JW Pharmaceutical announced that the dyslipidemia treatment pitavastatin and ezetimibe : Rivarojet) held a symposium on combination therapy and received high interest from medical staff and pharmaceutical industry officials. At this symposium, Professor Jun-Hwa Hong of the Department of Endocrinology at Eulji University Hospital was the presenter.
With an estimated 10 million dyslipidemia patients in Korea, the statin formulation used as a standard treatment for dyslipidemia has no major side effects and has been consistently used for the past 30 years due to its excellent effectiveness.
In particular, statins are excellent for lowering LDL cholesterol levels and have the effect of lowering the overall incidence of cardiovascular diseases, so various types of drugs have been commercialized in the market. However, there is a concern that it is always followed like a tag, and that is the risk associated with diabetes (NODM, New-Onset Diabetes Mellitus).
# Diabetes risk (NODM) and statin medications
The JUPITER clinical study published in NEJM in 2008 was a large-scale clinical trial conducted by the American Heart Association with 8,900 patients. appear.
In addition, a meta-analysis-related study published in The Lancet in 2010 increased the risk of diabetes by 9% when taking statins. According to a paper published in JAMA in 2011, high-dose statin therapy resulted in 12% higher NODM compared to low-dose.
As research on statins and the risk of developing diabetes (NODM) continued, concerns continued. The phrase was added as a warning to the statin product label.
Diabetes mellitus, like high blood pressure, can cause various complications, so special attention is required. In particular, patients with diabetes and pre-diabetes are more likely to develop cardiovascular disease than other patients, so they should keep their LDL cholesterol target lower.
In fact, among the ‘pre-diabetic’ patients with fasting blood sugar of 100 to 125 mg/dL or higher, dyslipidemia was present in regarding half, and in the case of diabetic patients, the ratio of LDL cholesterol levels of 100 mg/dL or higher was close to 50%. In other words, a significant number of pre-diabetes and diabetic patients suffer from dyslipidemia as a comorbidity.
In Korea, the cardiovascular risk assessment of the dyslipidemia treatment guidelines classifies diabetic patients as a ‘high-risk group’ and recommends that their target LDL cholesterol level be less than 100 mg/dL.
In order to reach lower LDL cholesterol levels, high doses of statins must be used.
# Pitabastatin, NODM safety ‘superior’ compared to other formulations
‘Pitavastatin (item name: Livaro)’ is the background to attract attention as a treatment option for dyslipidemia. Pitavastatin is effective even at a lower dose than other options and has been proven to be safe.
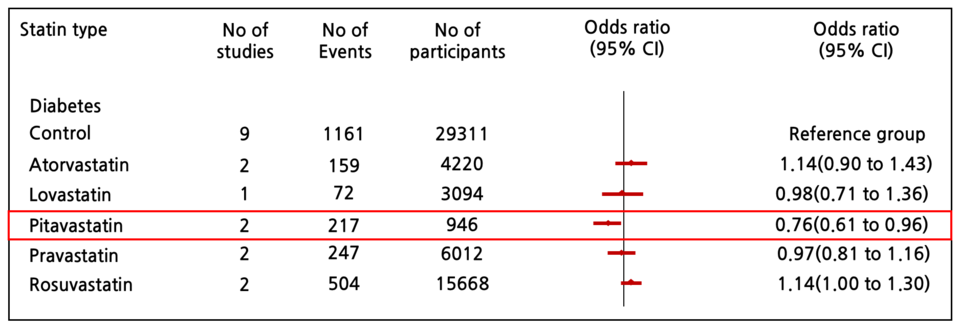
In a ‘statin drug-related meta-analysis study’ published in the British Medical Journal (BMJ) in 2021, the risk of developing diabetes according to the statin option was measured in 12,456 patients who had never had cardiovascular disease before. Pitavastatin was administered to the experimental group, and atorvastatin, lovastatin, pravastatin, and rosuvastatin were used in the control group.
As a result of the analysis, the experimental group (pitavastatin) significantly reduced the risk of diabetes (24%↓) compared to the control group, compared to atorvastatin by 51% (HR=1.49, 95% CI 1.08 to 2.05), and by 50% compared to rosuvastatin (HR=1.50, 95% CI 1.16 to 1.94) The risk was low.
However, in actual clinical practice, when low-dose statin monotherapy is used, there are cases in which the LDL cholesterol level does not sufficiently reach the target in the high-risk group and the ultra-high-risk group.
According to the data analyzed by the National Health Insurance Corporation on 510 thousand patients with dyslipidemia in Korea, the rate of achieving the target LDL-C of less than 70 mg/dL in high-risk patients is 10 to 20% of the total, and diabetes patients also was found to be similar.
# Pitavastatin and ezetimibe combination therapy, which is spotlighted in high-risk and ultra-high-risk groups
When statins alone are insufficient to reduce lipids, additional options are needed to solve this problem.
In the IMPROVE-IT study published in NEJM in 2015, LDL-LDL between statin monotherapy and statin-ezetimibe combination therapy in 18,144 hospitalized patients who were stabilized within 10 days for acute coronary syndrome (ACS). -C level control was compared.
As a result, ezetimibe combination therapy not only additionally decreased LDL-C levels compared to statin monotherapy, but also significantly reduced the incidence of cardiovascular events. After a total of 7 years of follow-up, the number of cardiovascular events was 2,742 cases with statin monotherapy and 2572 cases with ezetimibe combination therapy, which was 6.4% lower.
After the publication of the IMPROVE-IT clinical trial, European guidelines strongly recommended ezetimibe combination therapy. In the 2011 guideline, combination therapy was ‘may be considered’ if the LDL-C target was not reached, but the 2016 guideline changed to ‘should be considered’.
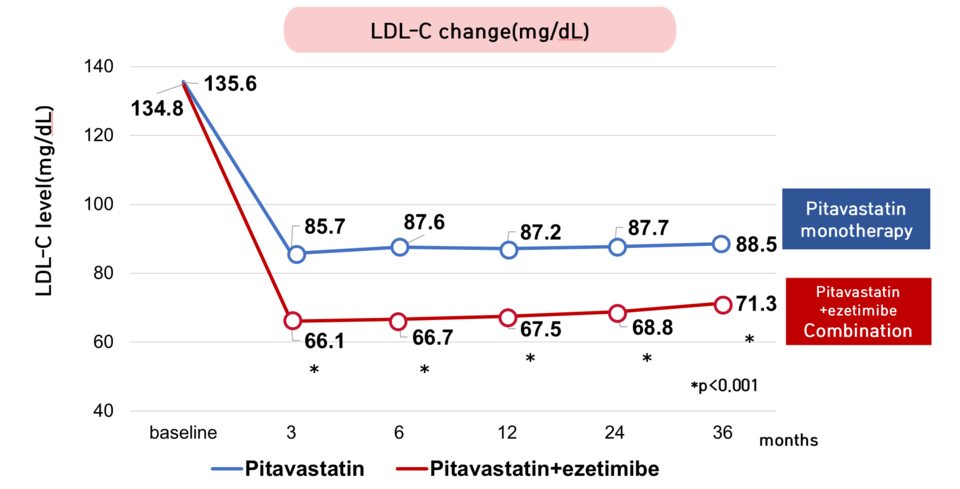
Later, in the HIJ-PROPER clinical trial published in 2017, the difference between the pitavastatin single drug (item name: Rivaro) and the pitavastatin/ezetimibe combination (item name: Rivarozet) was compared, and the results were similar to those of the IMPROVE-IT study. did. The combined treatment showed a significant LDL-C reduction effect compared to the single treatment.
As a result of follow-up of 1734 patients with acute coronary syndrome (ACS) and dyslipidemia for an average of 3.86 years, the LDL-C level in the single drug group was maintained at 85-89 mg/dL from 3 months following administration. and the combination drug group was found to be 66 to 71 mg/dL. Combination therapy showed superior LDL-C lowering effect than monotherapy.
Next, there was no significant difference in the incidence of cardiovascular events between the two groups, but a sub-comparison of patients with poor lipid management with LDL-C levels of 131 mg/dL or higher showed that the combination therapy had a 28% increase in the incidence of cardiovascular disease compared to the monotherapy. was regarding low
Recently, the need for more active LDL-C level management has been emphasized in the treatment of dyslipidemia, and especially considering the high risk of cardiovascular disease in prediabetes and diabetic patients, it is necessary to develop a therapeutic agent with less effect on blood sugar and excellent lipid-lowering effect. It seems desirable to prioritize.

